The immune system is a vital defense mechanism that protects the body from infections, diseases, and foreign invaders. For the NCLEX-RN® Exam, understanding immune-related concepts such as innate and adaptive immunity, hypersensitivity reactions, autoimmune disorders, and immunodeficiency is essential. Nurses play a critical role in assessing, managing, and educating patients about immune system disorders while prioritizing infection prevention. Mastery of nursing interventions, pharmacological treatments, and patient safety measures ensures optimal care and prepares you to excel in immune-related NCLEX-RN® questions.
Learning Objectives
In studying “Adult Health: Immune” for the NCLEX-RN® Exam, you should learn to understand the immune system’s role in defending against pathogens and maintaining homeostasis. Explore key concepts such as innate and adaptive immunity, hypersensitivity reactions, and autoimmune and immunodeficiency disorders. Evaluate clinical manifestations, diagnostic findings, and nursing interventions for immune-related conditions like anaphylaxis, HIV/AIDS, and rheumatoid arthritis. Analyze pharmacological treatments, including immunosuppressants and vaccines, and their nursing implications. Additionally, apply infection control measures, patient education strategies, and prioritize care for immunocompromised individuals to interpret clinical scenarios and demonstrate critical thinking in NCLEX practice questions.
1. Introduction of Immune System
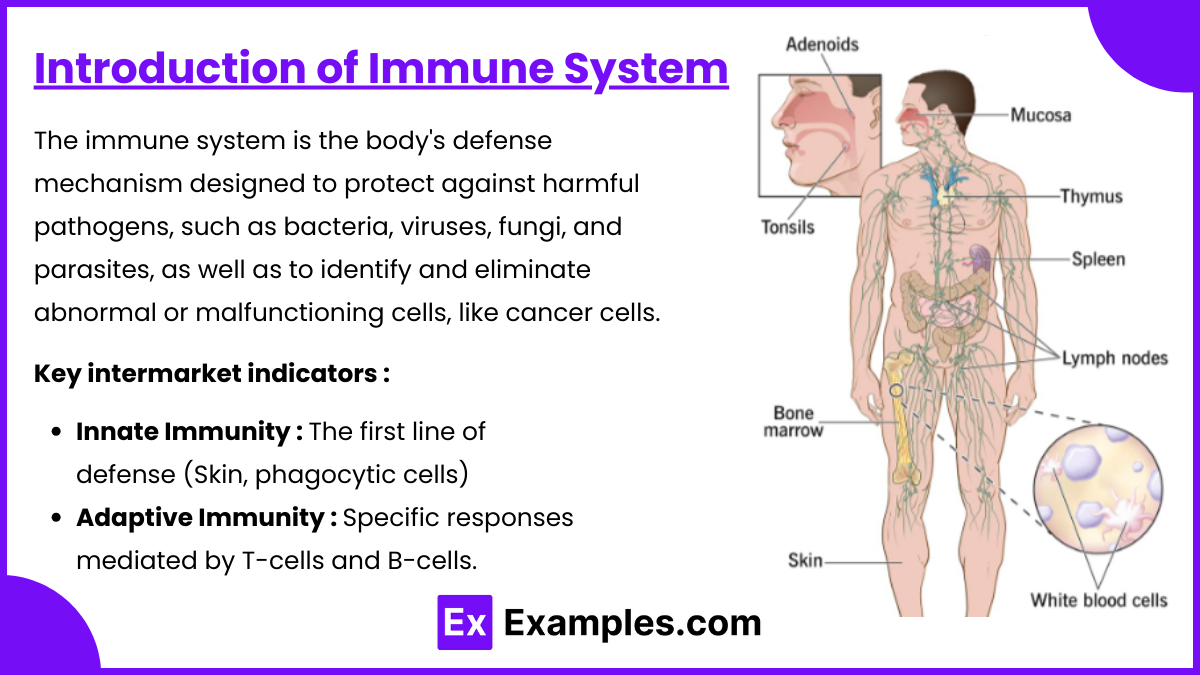
The immune system is the body’s defense mechanism designed to protect against harmful pathogens, such as bacteria, viruses, fungi, and parasites, as well as to identify and eliminate abnormal or malfunctioning cells, like cancer cells. It is composed of specialized cells, tissues, and organs that work together to detect and neutralize threats while maintaining the body’s overall health and stability.
Components of the Immune System
- Innate Immunity: The first line of defense (e.g., skin, mucous membranes, phagocytic cells, natural killer cells).
- Adaptive Immunity: Specific responses mediated by T-cells and B-cells.
- Humoral Immunity: Involves B-cells producing antibodies.
- Cell-Mediated Immunity: Involves T-cells attacking infected or abnormal cells.
2. Immune Responses
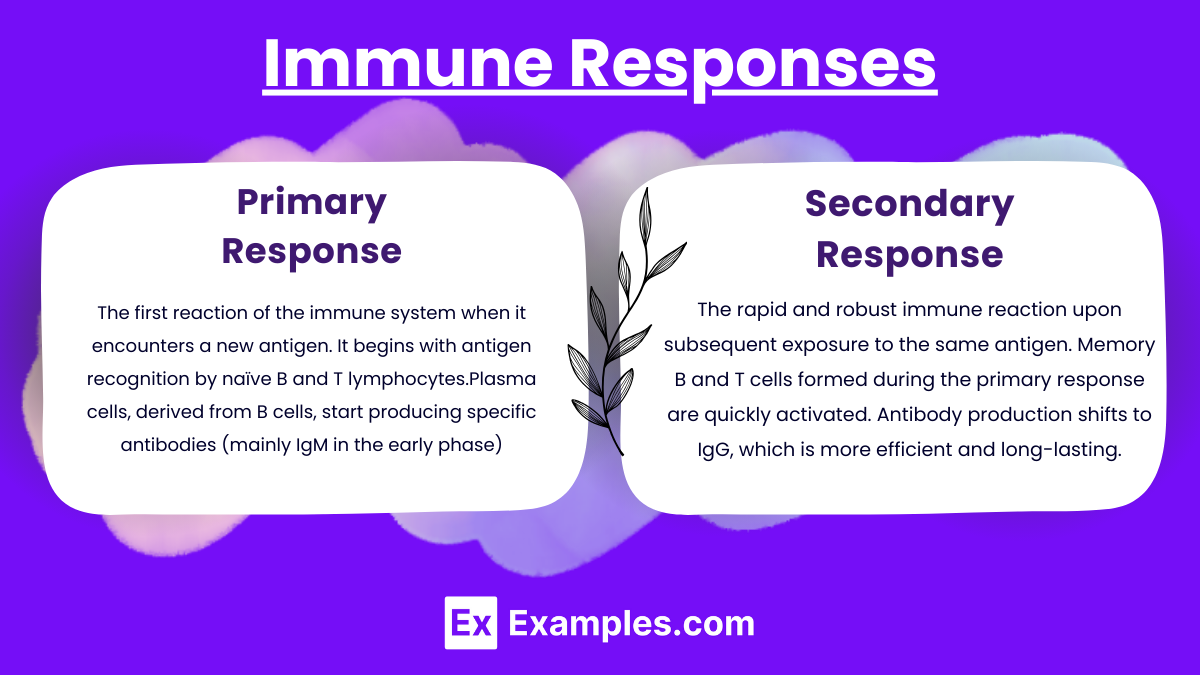
The immune response is the body’s coordinated reaction to foreign substances (antigens) to protect and maintain homeostasis. This response involves both innate and adaptive immunity and is divided into two major types:
- Primary Response: The first reaction of the immune system when it encounters a new antigen. It begins with antigen recognition by naïve B and T lymphocytes.Plasma cells, derived from B cells, start producing specific antibodies (mainly IgM in the early phase).Activation of T cells results in the production of cytokines and cytotoxic effects on infected cells.
- Characteristics:
- Slow onset (typically 7–10 days for a peak response).
- Involves a smaller magnitude of antibody production.
- Creates memory cells for future recognition of the same antigen.
- Secondary Response: The rapid and robust immune reaction upon subsequent exposure to the same antigen. Memory B and T cells formed during the primary response are quickly activated. Antibody production shifts to IgG, which is more efficient and long-lasting. Faster proliferation and activation of effector cells.
- Characteristics:
- Faster onset (1–3 days).
- Higher magnitude of antibody production.
- Enhanced specificity and efficiency in eliminating the antigen.
3. Common Immune Disorders
- Autoimmune Diseases: Autoimmune diseases are conditions in which the immune system mistakenly attacks the body’s own healthy tissues, perceiving them as foreign. This abnormal response causes inflammation and damage to various organs and systems. Common examples include rheumatoid arthritis, lupus, multiple sclerosis, and type 1 diabetes, each affecting specific or multiple body parts.
- Systemic Lupus Erythematosus (SLE): Chronic inflammation; monitor for butterfly rash, fatigue, and joint pain.
- Rheumatoid Arthritis (RA): Immune-mediated joint inflammation; assess for morning stiffness and nodules.
- Immunodeficiency Disorders: Immunodeficiency Disorders are conditions where the immune system’s ability to fight infections and diseases is compromised or entirely absent.
- Primary: Congenital, e.g., Severe Combined Immunodeficiency (SCID).
- Secondary: Acquired, e.g., HIV/AIDS.
- NCLEX Focus: Opportunistic infections like Kaposi’s sarcoma, pneumocystis pneumonia.
- Hypersensitivity Reactions: Hypersensitivity Reaction is an exaggerated or inappropriate immune response to a harmless antigen, leading to tissue damage or disease.
- Anaphylaxis: Recognize signs (dyspnea, hives, hypotension); administer epinephrine IM promptly.
4. Nursing Management
- Interventions:
- Administer immunizations and educate about schedules.
- Monitor for infection signs: fever, redness, drainage.
- Educate on infection prevention: hand hygiene, avoiding crowds for immunosuppressed patients.
- Provide care for patients undergoing immunosuppressive therapy (e.g., organ transplant recipients).
Examples
Example 1. Systemic Lupus Erythematosus (SLE)
A 32-year-old female presents with fatigue, joint pain, and a butterfly-shaped rash on her face. Laboratory results show positive antinuclear antibodies (ANA) and elevated erythrocyte sedimentation rate (ESR), confirming systemic lupus erythematosus. As the nurse, prioritize interventions such as monitoring for renal involvement (e.g., proteinuria), educating the patient to avoid sun exposure, and administering prescribed corticosteroids and immunosuppressants. NCLEX focus: Recognizing signs of exacerbation and teaching self-care measures.
Example 2. Anaphylaxis
A 45-year-old male is admitted to the emergency department after eating peanuts. He exhibits dyspnea, facial swelling, and hypotension. Recognize these as signs of anaphylaxis and implement immediate interventions, including administering epinephrine intramuscularly, maintaining airway patency, and starting IV fluids to treat hypotension. NCLEX focus: Prompt identification and prioritization of life-saving measures.
Example 3. HIV/AIDS
A 50-year-old male with a history of HIV presents with fever, weight loss, and a persistent cough. CD4 count is 150 cells/mm³, and a chest X-ray reveals infiltrates, indicating pneumocystis pneumonia. Nursing care includes administering antiretroviral therapy (ART), monitoring for opportunistic infections, and educating the patient on adherence to ART and infection prevention. NCLEX focus: Infection control, patient education, and monitoring therapeutic response to medications.
Example 4. Rheumatoid Arthritis (RA)
A 60-year-old female reports morning stiffness lasting over an hour, swollen joints, and difficulty performing daily activities. Diagnosed with rheumatoid arthritis, the patient begins treatment with disease-modifying antirheumatic drugs (DMARDs). Nursing interventions include teaching the importance of medication adherence, applying heat or cold packs for symptom relief, and encouraging gentle exercises to maintain joint mobility. NCLEX focus: Non-pharmacological interventions and patient education on chronic disease management.
Example 5. Post-Transplant Immunosuppression
A 55-year-old male who underwent a kidney transplant is prescribed tacrolimus to prevent organ rejection. He reports mild fever and fatigue, raising concern for infection due to immunosuppressive therapy. Nursing care involves close monitoring for signs of infection, ensuring the patient avoids large crowds, and reinforcing adherence to lifelong immunosuppressant therapy. NCLEX focus: Early recognition of complications and prevention of rejection or infection.
Practice Questions
Question 1
A patient experiencing an anaphylactic reaction is brought to the emergency department. Which action should the nurse perform first?
A. Administer oxygen at 6 L/min via nasal cannula.
B. Start an IV infusion of normal saline.
C. Administer epinephrine intramuscularly.
D. Place the patient in a supine position.
Answer: C. Administer epinephrine intramuscularly
Explanation: In an anaphylactic reaction, epinephrine is the first-line treatment as it counteracts severe hypotension, bronchospasm, and airway obstruction by stimulating alpha and beta-adrenergic receptors. Administering epinephrine intramuscularly (IM) in the mid-thigh ensures rapid absorption and action.
- Other Options:
- A. Administer oxygen: Oxygen is important but not the immediate first action; it supports breathing after the airway is managed.
- B. Start IV fluids: IV fluids help treat hypotension caused by vasodilation, but epinephrine is prioritized to stop the reaction.
- D. Supine position: Positioning is beneficial to maintain perfusion but does not address the immediate cause of anaphylaxis.
Question 2
A nurse is educating a patient newly diagnosed with systemic lupus erythematosus (SLE). Which statement by the patient indicates a need for further teaching?
A. “I should use sunscreen when I go outside.”
B. “I will monitor for unusual fatigue and joint pain.”
C. “I can stop taking my medications once I feel better.”
D. “I should notify my doctor if I develop a fever.
Answer: C. “I can stop taking my medications once I feel better.”
Explanation: SLE is a chronic autoimmune condition requiring long-term treatment to manage symptoms and prevent flare-ups. Stopping medications without a healthcare provider’s guidance can result in exacerbations of the disease.
- Other Options:
- A. Use sunscreen: Essential because SLE increases photosensitivity.
- B. Monitor fatigue and joint pain: These are common symptoms, and monitoring them helps manage disease progression.
- D. Notify doctor of fever: Fever can indicate an infection or disease flare, which requires prompt attention.
Question 3
A patient with HIV is admitted with a CD4+ count of 180 cells/mm³. Which nursing intervention is the highest priority?
A. Monitor for signs of opportunistic infections.
B. Administer pneumococcal and influenza vaccines.
C. Educate the patient on safe sexual practices.
D. Provide emotional support to reduce stress levels.
Answer: A. Monitor for signs of opportunistic infections
Explanation: A CD4+ count below 200 cells/mm³ indicates a severely weakened immune system and places the patient at high risk for opportunistic infections (e.g., Pneumocystis jirovecii pneumonia, candidiasis). Early identification and treatment of infections are critical to improving outcomes.
- Other Options:
- B. Administer vaccines: Important but not the immediate priority when opportunistic infections are a risk.
- C. Educate on safe practices: Important for preventing disease transmission but secondary to addressing life-threatening complications.
- D. Emotional support: Important but not as urgent as monitoring for infections.