Child Health: Immune refers to the state and function of the immune system in children, which is crucial for defending against infections, maintaining homeostasis, and identifying harmful pathogens. In infancy, immunity relies on passive maternal antibodies, gradually transitioning to active immunity as the child grows. The immune system includes innate defenses (e.g., skin, mucosa) and adaptive mechanisms (e.g., B and T lymphocytes). Pediatric immune health encompasses preventing infections through vaccinations, identifying immune-related disorders, and managing autoimmune conditions, hypersensitivities, or immunodeficiencies with appropriate interventions.
Learning Objectives
In studying “Child Health: Immune” for the NCLEX-RN® exam, you should learn to understand the development and function of the pediatric immune system, including innate and adaptive immunity. Evaluate the clinical presentation and nursing management of common immune disorders such as primary immunodeficiencies, autoimmune diseases, and hypersensitivity reactions. Analyze the principles of immunization schedules, contraindications, and patient education. Additionally, explore how immune responses influence infection control, vaccination, and allergy management in children. Apply your understanding to prioritize care, ensure patient safety, and interpret clinical scenarios in NCLEX-style practice questions involving immune health in pediatric populations.
Immune System Basics
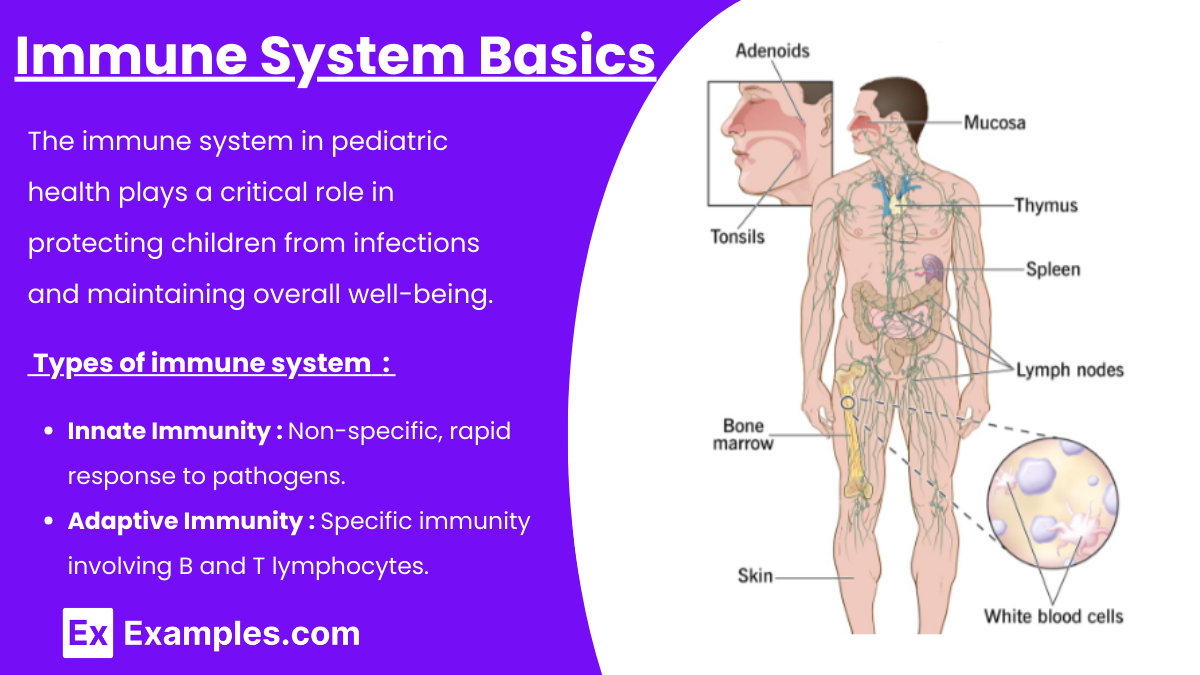
The immune system in pediatric health plays a critical role in protecting children from infections and maintaining overall well-being. Given the immaturity of the immune system in infants and young children, they are particularly vulnerable to infections, autoimmune disorders, and hypersensitivity reactions. For the NCLEX-RN®, understanding pediatric immune disorders, vaccination schedules, and nursing interventions is essential to provide safe, effective care. The immune system is divided into two main types:
- Innate Immunity:
- First line of defense (e.g., skin, mucous membranes, inflammatory response).
- Non-specific, rapid response to pathogens.
- Adaptive Immunity:
- Specific immunity involving B and T lymphocytes.
- Develops over time through exposure to antigens or immunizations.
In children, the immune system matures gradually, with the first few months relying on maternal antibodies (IgG) passed through the placenta and breastmilk.
Immune System Disorders in Pediatrics
1. Primary Immunodeficiency Disorders (PIDs)
- Congenital disorders caused by genetic defects affecting the immune system.
- Common examples:
- Severe Combined Immunodeficiency (SCID): Absence of both B and T cells, leading to severe vulnerability to infections.
- Wiskott-Aldrich Syndrome: X-linked disorder with eczema, thrombocytopenia, and recurrent infections.
- X-linked Agammaglobulinemia (Bruton’s Disease): Absence of mature B cells, leading to recurrent bacterial infections.
Nursing Focus:
- Ensure infection control measures (hand hygiene, isolation as needed).
- Administer immunoglobulin therapy (IVIG) or stem cell transplants if indicated.
- Educate families about avoiding exposure to pathogens and early recognition of infections.
2. Hypersensitivity Reactions
- Abnormal immune responses to antigens.
- Types of Hypersensitivity:
- Type I (Immediate): Allergies, anaphylaxis.
- Type II (Cytotoxic): Hemolytic disease of the newborn.
- Type III (Immune Complex): Serum sickness.
- Type IV (Delayed): Contact dermatitis, transplant rejection.
Nursing Focus:
- For anaphylaxis:
- Administer epinephrine, oxygen, and antihistamines.
- Monitor airway patency and hemodynamic stability.
- Educate families about allergen avoidance and emergency preparedness (e.g., EpiPen use).
3. Autoimmune Disorders
- The immune system attacks its own tissues.
- Common examples:
- Juvenile Idiopathic Arthritis (JIA): Chronic inflammation of joints.
- Systemic Lupus Erythematosus (SLE): Multi-system autoimmune disease.
Nursing Focus:
- Administer anti-inflammatory medications (NSAIDs, corticosteroids).
- Educate on lifestyle adaptations (e.g., maintaining physical activity, avoiding sun exposure in SLE).
- Monitor for signs of disease exacerbation.
4. Human Immunodeficiency Virus (HIV) in Children
- Pathophysiology:
- HIV targets CD4+ T cells, compromising adaptive immunity.
- Transmission:
- Vertical (mother to child), transfusions, or breastfeeding.
- Clinical Manifestations:
- Recurrent infections, failure to thrive, developmental delays.
Nursing Focus:
- Promote antiretroviral therapy adherence.
- Monitor growth, development, and opportunistic infections.
- Provide nutritional support and immunizations as indicated (avoid live vaccines).
Immunizations
Immunizations refer to the process by which a person is made resistant or immune to an infectious disease, typically through the administration of a vaccine. Vaccines stimulate the body’s immune system to recognize and fight pathogens such as bacteria or viruses, preventing illness or reducing its severity.
1. Importance: Vaccination is a cornerstone of pediatric immune system health, preventing life-threatening infections.
2. Recommended Schedule (CDC):
- Birth: Hepatitis B (HepB).
- 2, 4, 6 months: DTaP, Hib, IPV, PCV, RV.
- 12-15 months: MMR, Varicella, HepA.
- 4-6 years: Booster doses for DTaP, IPV, MMR, Varicella.
3. Nursing Role in Vaccination:
- Assess for contraindications (e.g., allergies, immunocompromised status).
- Educate parents on vaccine safety and common side effects.
- Monitor for adverse reactions such as fever or localized swelling.
4. Common Vaccine-Preventable Diseases:
- Measles: High fever, Koplik spots, rash.
- Pertussis: Severe cough, risk of apnea in infants.
- Tetanus: Muscle spasms, lockjaw.
- Polio: Paralysis and muscle weakness.
Nursing Management of Immune-Related Conditions
1. General Interventions : General Interventions in the nursing management of immune-related conditions focus on minimizing infection risks and promoting overall health. Nurses should assess patients for signs of infection, such as fever, lethargy, or irritability, and implement strategies to enhance immune function, including ensuring proper nutrition.
- Assess for signs of infection (fever, lethargy, irritability).
- Ensure proper nutrition to support immune function.
- Maintain strict hand hygiene and infection control measures.
2. Medications : Medications play a critical role in managing immune-related conditions. Immunoglobulin therapy (IVIG) is commonly used to treat primary immunodeficiency disorders (PIDs) and Kawasaki disease by boosting passive immunity. Corticosteroids are effective in controlling inflammation in autoimmune conditions, while antiretrovirals are essential for managing HIV by suppressing viral replication.
- Immunoglobulin Therapy (IVIG): For PIDs or Kawasaki Disease.
- Corticosteroids: To manage inflammation in autoimmune conditions.
- Antiretrovirals: For managing HIV.
- Epinephrine: First-line treatment for anaphylaxis.
3. Education : Education is a cornerstone of nursing care, emphasizing the importance of infection prevention strategies. Families should be informed about adhering to vaccination schedules, practicing proper hand hygiene, and avoiding crowded places during disease outbreaks to minimize exposure risks. Providing comprehensive education empowers patients and their families to effectively manage immune-related conditions and improve overall health outcomes.
- Teach families about infection prevention strategies:
- Vaccination schedules.
- Proper hand hygiene.
- Avoiding crowded places during outbreaks.
Examples
Example 1. Severe Combined Immunodeficiency (SCID):
A 4-month-old infant presents with recurrent respiratory infections, persistent diarrhea, and failure to thrive. The infant has a family history of early childhood deaths due to infections. Laboratory findings show an absence of T and B lymphocytes. The nurse recognizes this as SCID, a primary immunodeficiency disorder. Priority interventions include infection prevention, administration of intravenous immunoglobulin (IVIG), and preparing the family for possible hematopoietic stem cell transplantation. Educating the parents about strict infection control measures at home is crucial.
Example 2. Juvenile Idiopathic Arthritis (JIA)
A 10-year-old child is brought to the clinic with complaints of morning joint stiffness and swelling in the knees and wrists. The child reports fatigue and occasional low-grade fever. The nurse suspects JIA, an autoimmune condition affecting children. Nursing interventions focus on pain management through NSAIDs, physical therapy to maintain joint function, and educating the family about recognizing flare-ups. The nurse also discusses strategies to promote school attendance and support the child’s psychosocial development.
Example 3. Anaphylaxis After Peanut Ingestion:
A 7-year-old child is rushed to the emergency department with difficulty breathing, facial swelling, and hives after accidentally consuming peanuts. The nurse identifies this as an anaphylactic reaction and immediately administers intramuscular epinephrine. Oxygen is provided via a face mask, and the child is closely monitored for airway obstruction and shock. The nurse educates the family about allergen avoidance, how to use an epinephrine auto-injector, and the importance of carrying it at all times.
Example 4. Human Immunodeficiency Virus (HIV) in a Child:
A 6-year-old with vertically transmitted HIV presents for a routine check-up. The child is currently on antiretroviral therapy (ART) and has a stable CD4 count. The nurse assesses the child’s growth and development, monitors for signs of opportunistic infections, and reinforces adherence to ART. The nurse also educates the family on ensuring a balanced diet, maintaining proper hygiene, and the importance of regular follow-ups. Special emphasis is placed on avoiding live vaccines unless directed by the healthcare provider.
Example 5. Measles in an Unvaccinated Child:
A 3-year-old who has not received routine vaccinations presents with high fever, cough, conjunctivitis, and a red, blotchy rash starting on the face and spreading downward. The nurse recognizes these as classic signs of measles, a preventable viral infection. Interventions include supportive care such as antipyretics for fever, hydration, and isolating the child to prevent the spread of infection. The nurse educates the parents about the importance of vaccination and schedules follow-up appointments to catch up on missed vaccines once the child recovers.
Practice Questions
Question 1
A 4-year-old child with Severe Combined Immunodeficiency (SCID) is admitted for recurrent infections. What is the nurse’s priority intervention?
A. Administer prophylactic antibiotics as prescribed.
B. Educate the parents on proper hand hygiene techniques.
C. Prepare the child for a hematopoietic stem cell transplant.
D. Place the child in a protective isolation room.
Answer: D. Place the child in a protective isolation room.
Explanation: Children with SCID have severely compromised immune systems, making them highly susceptible to infections. Protective isolation minimizes exposure to pathogens and is the priority intervention to prevent life-threatening infections. While A (administering antibiotics) and B (teaching hand hygiene) are critical aspects of care, they do not directly address immediate risk. C (preparing for transplant) is essential but does not take precedence over protecting the child from infections.
Question 2
A child with a peanut allergy begins to exhibit wheezing, facial swelling, and hives after accidentally ingesting peanut butter. What is the nurse’s priority action?
A. Administer oxygen via face mask.
B. Administer epinephrine intramuscularly.
C. Start an intravenous line for fluid resuscitation.
D. Monitor the child’s vital signs.
Answer: B. Administer epinephrine intramuscularly.
Explanation: This child is experiencing anaphylaxis, a life-threatening allergic reaction. The first-line treatment is intramuscular epinephrine, which helps reverse airway constriction and stabilize the cardiovascular system. A (administering oxygen) and C (starting an IV line) are important but secondary to epinephrine administration. D (monitoring vital signs) is part of ongoing assessment but does not address the immediate issue. Prioritization follows the ABCs (Airway, Breathing, Circulation) framework.
Question 3
The parents of a 12-month-old child ask why their child should receive the measles, mumps, and rubella (MMR) vaccine. Which response by the nurse is most appropriate?
A. “It will prevent your child from getting these diseases and their complications.”
B. “It is a state requirement before your child can attend school.”
C. “It ensures herd immunity in your community.”
D. “It eliminates the risk of your child developing an allergic reaction to these diseases.”
Answer: A. “It will prevent your child from getting these diseases and their complications.”
Explanation: The most appropriate response emphasizes the benefits to the child, including preventing serious complications such as pneumonia (measles), orchitis (mumps), and congenital rubella syndrome (if exposed during pregnancy later in life). B (state requirements) and C (herd immunity) are accurate but do not directly address the parents’ concern. D is incorrect because vaccines do not eliminate the risk of an allergic reaction but rather reduce the likelihood of contracting the disease.