Infectious diseases are a critical focus in the NCLEX RN® exam, assessing a nurse’s ability to prevent, manage, and control conditions caused by bacteria, viruses, fungi, and parasites. These diseases often present challenges like rapid spread, severe complications, and resistance to treatment. The exam emphasizes key concepts, including pathophysiology, isolation precautions, vaccination, and antimicrobial therapies. Nurses must prioritize patient safety, infection prevention, and evidence-based interventions while managing conditions like pneumonia, tuberculosis, sepsis, and HIV/AIDS, ensuring optimal care and preventing further transmission.
Learning Objectives
In studying “Infectious Disease” for the NCLEX RN® exam, you should learn to understand the pathophysiology, transmission, and clinical manifestations of common infections, including pneumonia, tuberculosis, and sepsis. Analyze the principles of infection control, including isolation precautions and hand hygiene. Evaluate treatment protocols such as antimicrobial therapy and supportive care measures. Additionally, explore how vaccination and patient education play roles in infection prevention. Apply your understanding to prioritize care, manage complications, and interpret laboratory findings. Utilize critical thinking to answer NCLEX-style questions that assess your ability to provide safe, evidence-based nursing interventions for infectious diseases.
Infectious diseases in adult health encompass illnesses caused by microorganisms like bacteria, viruses, fungi, and parasites. They can lead to localized or systemic infections, significantly impacting patient health and requiring prompt, accurate nursing interventions. For the NCLEX RN® exam, knowledge of pathophysiology, isolation precautions, and patient-centered care is critical for achieving high scores and ensuring optimal patient outcomes.
1. Pathophysiology of Infectious Diseases
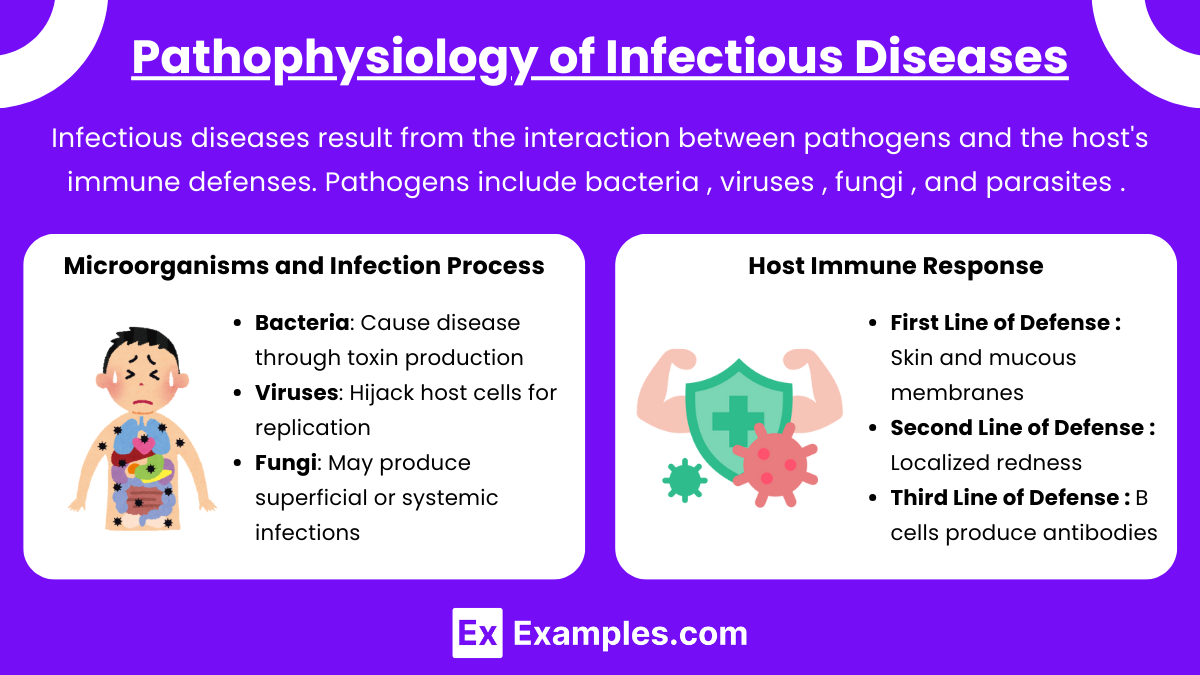
Infectious diseases result from the interaction between pathogens and the host’s immune defenses. Pathogens include bacteria (e.g., Staphylococcus aureus), viruses (e.g., Influenza virus), fungi (e.g., Candida albicans), and parasites (e.g., Plasmodium in malaria). The pathophysiology begins with pathogen entry, colonization, and evasion of host defenses.
Microorganisms and Infection Process:
- Bacteria: Cause disease through toxin production (e.g., endotoxins in E. coli) or direct tissue invasion.
- Viruses: Hijack host cells for replication, causing cytopathic effects (e.g., in herpesvirus infections).
- Fungi: May produce superficial (e.g., athlete’s foot) or systemic infections, particularly in immunocompromised individuals.
- Parasites: Utilize complex life cycles, often transmitted via vectors (e.g., mosquitos in malaria).
Host Immune Response:
- First Line of Defense:
- Physical Barriers: Skin and mucous membranes provide mechanical protection.
- Chemical Barriers: Enzymes in saliva, stomach acid, and antimicrobial peptides prevent pathogen growth.
- Second Line of Defense:
- Inflammatory Response: Localized redness, swelling, pain, and fever occur due to cytokines (e.g., interleukin-1, tumor necrosis factor-alpha).
- Phagocytosis: Neutrophils and macrophages engulf and destroy pathogens.
- Natural Killer (NK) Cells: Target and kill virus-infected or cancerous cells.
- Third Line of Defense:
- Humoral Immunity: B cells produce antibodies targeting specific antigens.
- Cell-Mediated Immunity: T cells (e.g., cytotoxic T cells) destroy infected cells and regulate immune responses.
- Memory Cells: Ensure a faster response to future infections by the same pathogen.
2. What are the types of infectious diseases?
Infectious diseases are illnesses caused by pathogenic microorganisms such as bacteria, viruses, fungi, parasites, or prions. These diseases can spread directly or indirectly between individuals, animals, or the environment. They are classified based on the type of pathogen causing the infection, the method of transmission, or the organ systems affected. Below is an overview of the main types of infectious diseases, explained in detail.
- Bacterial infections are caused by various species of bacteria, which are single-celled organisms. Common examples include tuberculosis (TB), urinary tract infections (UTIs), strep throat, and foodborne illnesses like Salmonella. These infections are often treated with antibiotics, though the rise of antibiotic resistance (e.g., methicillin-resistant Staphylococcus aureus or MRSA) poses a significant challenge. Bacterial infections can range from mild, such as ear infections, to life-threatening conditions like sepsis.
- Viral infections are caused by viruses, which are microscopic pathogens that invade and replicate inside the host’s cells. Examples include influenza, COVID-19 (caused by SARS-CoV-2), HIV/AIDS, hepatitis (A, B, and C), and measles. While many viral infections are self-limiting, some, like HIV and hepatitis, require long-term antiviral therapy. Vaccination has been a cornerstone in preventing many viral diseases, such as polio and rubella, reducing their global impact.
- Fungal infections are caused by fungi, which include yeasts and molds. These infections often affect the skin, mucous membranes, or lungs, particularly in immunocompromised individuals. Examples include candidiasis (e.g., oral thrush and vaginal yeast infections), ringworm (a type of tinea infection), and more severe diseases like aspergillosis and histoplasmosis. Antifungal medications are used to treat these infections, though prevention is crucial, particularly in hospital settings where fungal infections can spread.
- Parasitic infections occur when parasites, such as protozoa, helminths (worms), or ectoparasites, invade the body. Notable examples include malaria, caused by Plasmodium protozoa, giardiasis, toxoplasmosis, and schistosomiasis. Parasites can also cause skin infestations, such as scabies and lice. These infections may involve complex life cycles and often require specific antiparasitic treatments, along with measures to control the environmental spread of the parasite.
3. Common Adult Infectious Diseases
- Respiratory Infections
- Pneumonia:
- Pathogen: Streptococcus pneumoniae or viral agents.
- Symptoms: Fever, productive cough, dyspnea.
- Care: Oxygen therapy, antibiotics, incentive spirometry.
- NCLEX Tip: Prioritize oxygenation and infection control.
- Tuberculosis (TB):
- Pathogen: Mycobacterium tuberculosis.
- Symptoms: Chronic cough, hemoptysis, night sweats, weight loss.
- Isolation: Airborne precautions (negative pressure room, N95 mask).
- NCLEX Tip: Know Mantoux test interpretation and long-term medication compliance.
- Pneumonia:
- Urinary Tract Infections (UTIs)
- Common Cause: Escherichia coli.
- Symptoms: Dysuria, urinary urgency/frequency, hematuria.
- Nursing Care: Increase fluid intake, administer antibiotics, educate on hygiene.
- NCLEX Tip: Understand catheter-associated UTI (CAUTI) prevention.
- Gastrointestinal Infections
- Clostridioides difficile (C. diff):
- Symptoms: Severe diarrhea, abdominal pain.
- Isolation: Contact precautions.
- Treatment: Metronidazole or oral vancomycin.
- NCLEX Tip: Focus on hand hygiene with soap and water (not alcohol-based sanitizers).
- Hepatitis (A, B, C):
- Symptoms: Jaundice, fatigue, abdominal pain.
- Transmission: Hep A (fecal-oral), Hep B/C (bloodborne).
- Care: Rest, nutrition, antivirals (Hep B/C).
- Clostridioides difficile (C. diff):
- Bloodborne Infections
- HIV/AIDS:
- Symptoms: Opportunistic infections, wasting syndrome, Kaposi’s sarcoma.
- Care: Adherence to antiretroviral therapy (ART), infection prevention.
- NCLEX Tip: Know CD4 count significance and stages of infection.
- Sepsis:
- Definition: Systemic infection with organ dysfunction.
- Symptoms: Fever, tachycardia, hypotension, altered mental status.
- Care: IV antibiotics, fluids, vasopressors.
- HIV/AIDS:
- Skin and Soft Tissue Infections
- Cellulitis: Red, swollen, tender skin.
- Pathogen: Commonly Staphylococcus aureus or Streptococcus pyogenes.
- Treatment: Antibiotics, wound care.
- Sexually Transmitted Infections (STIs)
- Examples: Chlamydia, Gonorrhea, Syphilis.
- Symptoms: Discharge, pain, sores.
- NCLEX Tip: Emphasize safe sex education and partner notification.
Examples
Example 1: Pneumonia
This is a common respiratory infection caused by bacteria, viruses, or fungi, with Streptococcus pneumoniae being the most frequent bacterial cause. Patients present with symptoms such as fever, chills, productive cough, dyspnea, and pleuritic chest pain. Nursing care includes administering prescribed antibiotics, encouraging incentive spirometry, and monitoring oxygen saturation levels. Understanding chest X-ray findings and recognizing complications such as sepsis are critical for NCLEX RN® success.
Example 2: Tuberculosis (TB)
Caused by Mycobacterium tuberculosis, TB requires airborne precautions due to its transmission through respiratory droplets. Key symptoms include a persistent cough lasting more than three weeks, hemoptysis, night sweats, and weight loss. Nurses must prioritize isolation in a negative-pressure room and ensure strict compliance with antitubercular medications like isoniazid and rifampin. The NCLEX RN® often tests knowledge of PPD testing results, isolation protocols, and potential complications like latent TB reactivation.
Example 3: Sepsis
This life-threatening systemic infection occurs when the body’s response to an infection leads to organ dysfunction. Commonly arising from pneumonia, urinary tract infections, or surgical site infections, sepsis presents with fever, tachycardia, hypotension, and confusion. Nursing management includes administering IV fluids, broad-spectrum antibiotics, and monitoring for signs of septic shock. For NCLEX RN® questions, focus on identifying early symptoms and prioritizing interventions using the ABC framework (Airway, Breathing, Circulation).
Example 4: HIV/AIDS
This chronic condition is caused by the Human Immunodeficiency Virus (HIV) and leads to immune suppression and vulnerability to opportunistic infections. Patients may experience symptoms like fever, chronic diarrhea, weight loss, and opportunistic diseases such as Pneumocystis jirovecii pneumonia. Nursing responsibilities include educating patients on antiretroviral therapy adherence and managing infection prevention strategies. NCLEX RN® often evaluates understanding of disease progression, patient teaching, and opportunistic infection care.
Example 5: Urinary Tract Infections (UTIs)
These are commonly caused by Escherichia coli and affect the urinary system, leading to symptoms like dysuria, urinary frequency, urgency, and hematuria. Nursing interventions involve administering prescribed antibiotics, promoting hydration, and educating patients about prevention strategies, such as wiping front to back and avoiding irritants. On the NCLEX RN®, questions may focus on identifying risk factors for UTIs, such as catheter use, and recognizing signs of complications like pyelonephritis.
Practice Questions
Question 1
A 65-year-old client is admitted with pneumonia caused by Streptococcus pneumoniae. The nurse should prioritize which intervention?
A. Administer antipyretics as prescribed.
B. Monitor oxygen saturation levels continuously.
C. Encourage the client to rest and limit activity.
D. Educate the client on completing the antibiotic course.
Answer: B. Monitor oxygen saturation levels continuously.
Explanation: Maintaining adequate oxygenation is the top priority for a client with pneumonia. Oxygen saturation monitoring helps detect hypoxemia early, enabling timely intervention. While Options A, C, and D are important, they do not address the immediate need for ensuring oxygenation.
Question 2
A nurse is caring for a client with tuberculosis (TB) who has been prescribed isoniazid (INH). Which laboratory value requires immediate follow-up?
A. Hemoglobin level: 12 g/dL.
B. Platelet count: 180,000/mm³.
C. ALT (Alanine aminotransferase): 90 U/L.
D. Serum creatinine: 1.0 mg/dL.
Answer: C. ALT (Alanine aminotransferase): 90 U/L.
Explanation: Isoniazid can cause hepatotoxicity, and an elevated ALT level indicates liver injury or inflammation, necessitating immediate follow-up. The other values (Options A, B, and D) are within normal limits and are not directly affected by INH.
Question 3
A client is receiving treatment for sepsis. The nurse notes the following: temperature 101.5°F (38.6°C), heart rate 120 bpm, blood pressure 85/50 mmHg, and urine output 20 mL/hr. What is the nurse’s priority action?
A. Administer acetaminophen for the fever.
B. Start norepinephrine infusion as prescribed.
C. Increase the rate of IV fluid administration.
D. Notify the healthcare provider immediately.
Answer: C. Increase the rate of IV fluid administration.
Explanation: The client is showing signs of septic shock, and fluid resuscitation is the priority to restore intravascular volume and improve organ perfusion. While acetaminophen (Option A) may reduce fever, it does not address the hemodynamic instability. Norepinephrine (Option B) is often used after fluid resuscitation if hypotension persists. Notifying the provider (Option D) is necessary, but immediate fluid administration takes precedence.