Child Health: Infectious Disease is a critical topic for the NCLEX-RN® exam, focusing on the prevention, identification, and management of infections common in children. Due to their developing immune systems, children are particularly susceptible to illnesses like measles, chickenpox, pertussis, and scarlet fever. Nurses play a key role in recognizing symptoms, implementing isolation precautions, providing treatment, and educating families about vaccinations and infection prevention. Understanding pathophysiology, transmission, and nursing interventions ensures safe, effective care and reduces complications, promoting optimal outcomes in pediatric health.
Learning Objectives
In studying “Child Health: Infectious Disease” for the NCLEX-RN® exam, you should learn to understand the causes, transmission, and clinical presentations of common pediatric infectious diseases such as measles, chickenpox, pertussis, and scarlet fever. Analyze nursing interventions, including isolation precautions, symptom management, and medication administration. Evaluate the role of vaccinations in preventing disease outbreaks and complications. Additionally, explore how infection control strategies, patient education, and prioritization of care improve outcomes. Apply your understanding to interpret clinical scenarios, prioritize safety, and educate families effectively in NCLEX-style practice questions involving pediatric infectious diseases.
Common Pediatric Infectious Diseases
Children are particularly vulnerable to infectious diseases due to immature immune systems and frequent exposure in settings like schools and daycare. For the NCLEX-RN®, understanding infectious disease pathophysiology, prevention, nursing care, and patient education is critical. Mastering this topic helps prioritize safety, manage complications, and educate families effectively.
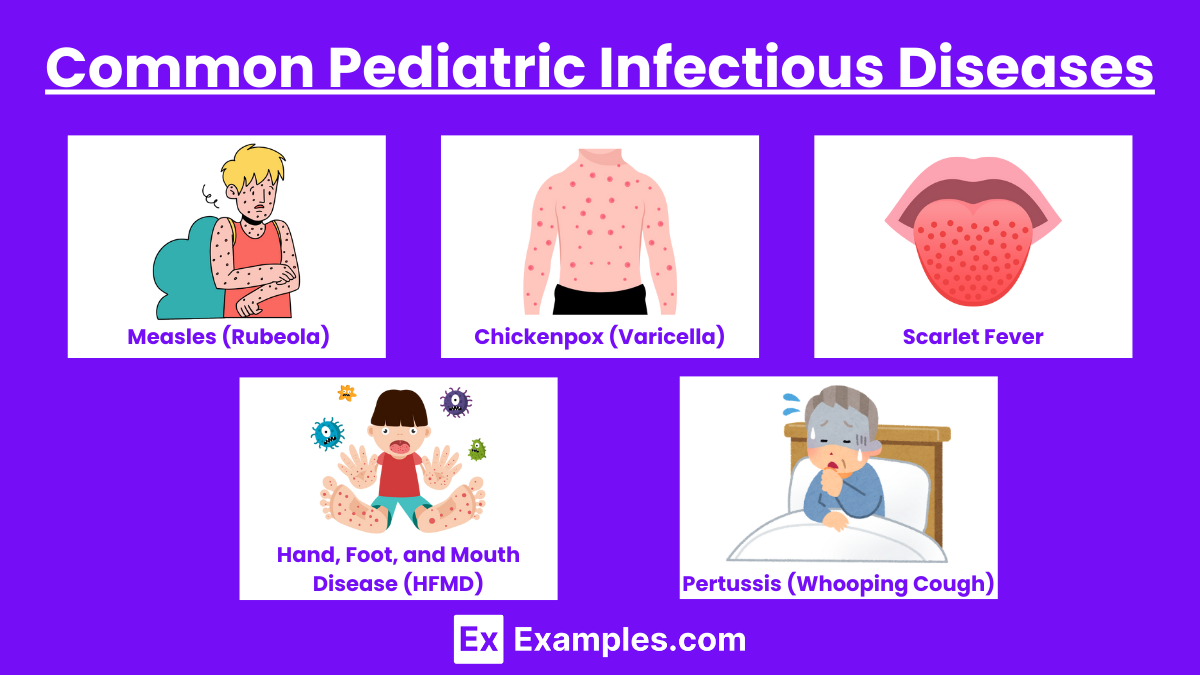
1. Measles (Rubeola)
- Cause: Measles virus.
- Transmission: Airborne droplets from coughs or sneezes of an infected person.
- Symptoms: Begins with fever, cough, runny nose, and conjunctivitis (the “3 C’s”). Koplik spots (white lesions inside the cheeks) appear, followed by a maculopapular rash starting at the hairline and spreading downward.
- Complications: Pneumonia, encephalitis, and death in severe cases.
- Nursing Care: Implement airborne precautions, provide supportive care (hydration, antipyretics), and educate on MMR vaccination to prevent future cases.
2. Chickenpox (Varicella)
- Cause: Varicella-zoster virus.
- Transmission: Direct contact with lesions, airborne droplets.
- Symptoms: Fever and malaise, followed by an itchy, vesicular rash that progresses to crusting lesions. Rash commonly starts on the trunk and spreads to the face and extremities.
- Complications: Secondary bacterial infections, pneumonia, encephalitis.
- Nursing Care: Airborne and contact precautions, antihistamines for itching, and acetaminophen for fever. Encourage vaccination to prevent the disease.
3. Scarlet Fever
- Cause: Group A Streptococcus (GAS).
- Transmission: Droplet transmission through respiratory secretions.
- Symptoms: High fever, sore throat, strawberry tongue, and a fine red rash with a sandpaper texture. The rash often peels after recovery.
- Complications: Rheumatic fever, glomerulonephritis.
- Nursing Care: Administer penicillin or amoxicillin, provide soft foods, and educate on completing the full course of antibiotics and infection prevention.
4. Hand, Foot, and Mouth Disease (HFMD)
- Cause: Coxsackievirus A16 or Enterovirus 71.
- Transmission: Fecal-oral and respiratory routes.
- Symptoms:
- Painful oral ulcers.
- Vesicular rash on hands, feet, and sometimes buttocks.
- Fever, irritability.
- Nursing Care:
- Symptom management: analgesics, antipyretics, hydration.
- Educate on hygiene practices to prevent transmission.
5. Pertussis (Whooping Cough)
- Cause: Coxsackievirus A16 or Enterovirus 71.
- Transmission: Fecal-oral and respiratory routes.
- Symptoms: Painful sores in the mouth, and a vesicular rash on the hands, feet, and sometimes the buttocks. Mild fever and irritability may accompany these symptoms.
- Complications: Dehydration due to painful oral sores.
- Nursing Care: Manage symptoms with analgesics, antipyretics, and encouraging hydration. Educate on proper hygiene to reduce transmission.
Nursing Management of Infectious Diseases
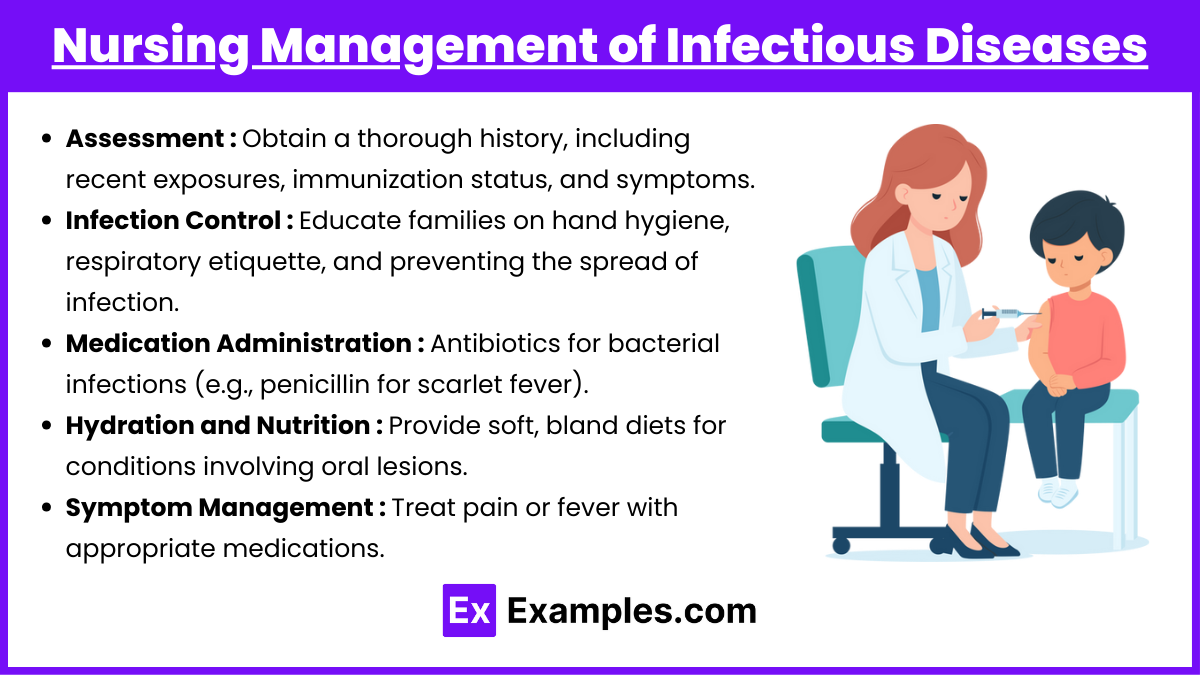
1. Assessment:
- Obtain a thorough history, including recent exposures, immunization status, and symptoms.
- Monitor for fever, rash, dehydration, and respiratory distress.
2. Infection Control:
- Implement appropriate isolation precautions:
- Airborne: Measles, chickenpox.
- Droplet: Pertussis, scarlet fever.
- Contact: HFMD.
- Educate families on hand hygiene, respiratory etiquette, and preventing the spread of infection.
3. Medication Administration:
- Antibiotics for bacterial infections (e.g., penicillin for scarlet fever).
- Antiviral medications for certain conditions (e.g., acyclovir for severe chickenpox).
- Antipyretics and analgesics for symptom relief (e.g., acetaminophen, ibuprofen).
4. Hydration and Nutrition:
- Encourage oral fluids to prevent dehydration, particularly in illnesses with fever or diarrhea.
- Provide soft, bland diets for conditions involving oral lesions.
5. Symptom Management:
- Address pruritus in conditions like chickenpox with antihistamines or soothing baths.
- Treat pain or fever with appropriate medications.
- Monitor for and address complications like secondary infections or respiratory distress.
Vaccination Guidelines for Pediatric Infectious Diseases
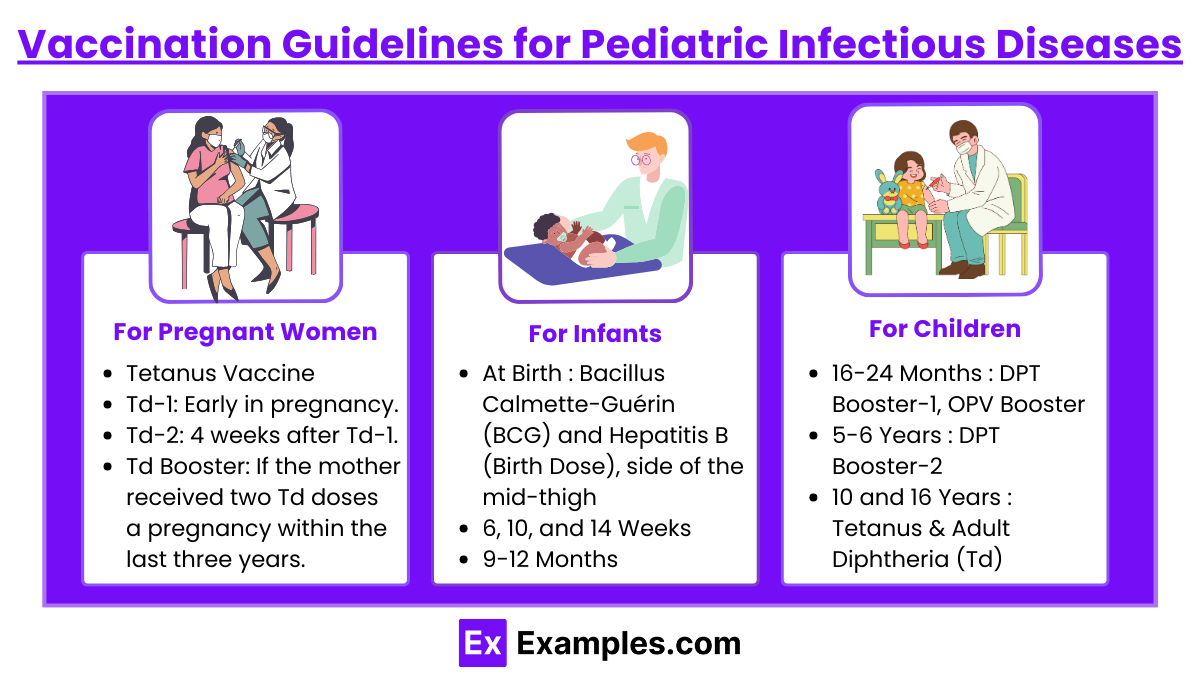
Ensuring timely and complete immunization is crucial for protecting children against various infectious diseases. In India, the Universal Immunization Programme (UIP) provides a comprehensive schedule for vaccinating infants, children, and pregnant women. Below is an overview of the vaccination guidelines:
For Pregnant Women:
- Tetanus & Adult Diphtheria (Td) Vaccine:
- Td-1: Early in pregnancy.
- Td-2: 4 weeks after Td-1.
- Td Booster: If the mother received two Td doses in a pregnancy within the last three years.
For Infants:
- At Birth:
- Bacillus Calmette-Guérin (BCG): Prevents tuberculosis; administered intradermally in the left upper arm.
- Hepatitis B (Birth Dose): Given within 24 hours of birth; intramuscular injection in the anterolateral side of the mid-thigh.
- Oral Polio Vaccine (OPV-0): Administered as 2 oral drops.
- 6, 10, and 14 Weeks:
- Pentavalent Vaccine (DPT + Hep B + Hib): Protects against diphtheria, pertussis, tetanus, hepatitis B, and Haemophilus influenzae type B; intramuscular injection in the anterolateral thigh.
- OPV 1, 2, 3: 2 oral drops at each visit.
- Fractional Inactivated Polio Vaccine (fIPV): Administered intradermally in the right upper arm at 6 and 14 weeks.
- Rotavirus Vaccine: 5 oral drops at each visit (where applicable).
- Pneumococcal Conjugate Vaccine (PCV): Intramuscular injection in the right anterolateral thigh at 6 and 14 weeks (where applicable).
- 9-12 Months:
- Measles/Rubella (MR) Vaccine: Subcutaneous injection in the right upper arm.
- Japanese Encephalitis (JE) Vaccine: Subcutaneous injection in the left upper arm (in endemic areas).
- Vitamin A (1st Dose): 1 ml (1 lakh IU) orally.
For Children:
- 16-24 Months:
- DPT Booster-1: Intramuscular injection in the left anterolateral thigh.
- OPV Booster: 2 oral drops.
- Measles/Rubella 2nd Dose: Subcutaneous injection in the right upper arm.
- JE 2nd Dose: Subcutaneous injection in the left upper arm (in endemic areas).
- Vitamin A (2nd Dose): 2 ml (2 lakh IU) orally; subsequent doses every 6 months up to 5 years of age.
- 5-6 Years:
- DPT Booster-2: Intramuscular injection in the upper arm.
- 10 and 16 Years:
- Tetanus & Adult Diphtheria (Td): Intramuscular injection in the upper arm at both ages.
Examples
Example 1. Measles (Rubeola)
A 4-year-old child presents with a high fever, cough, runny nose, conjunctivitis, and small white spots inside the cheeks (Koplik spots). Two days later, a red, blotchy rash appears on the face and spreads downward. The nurse prioritizes airborne isolation precautions to prevent transmission and provides supportive care, including antipyretics for fever and hydration. The family is educated on the importance of completing the MMR vaccine series to prevent future occurrences of measles and related complications, such as pneumonia or encephalitis.
Example 2. Pertussis (Whooping Cough)
A 6-month-old infant is admitted with severe, paroxysmal coughing fits followed by a high-pitched “whooping” sound and occasional cyanosis. The nurse implements droplet precautions and administers prescribed azithromycin to treat the infection. Oxygen therapy is provided to manage hypoxia, and the nurse closely monitors for signs of apnea. The parents are educated on completing the DTaP vaccination series and practicing proper hand hygiene to prevent transmission to others, especially vulnerable infants.
Example 3. Hand, Foot, and Mouth Disease (HFMD)
A 2-year-old child is brought to the clinic with a mild fever, painful oral ulcers, and a vesicular rash on the hands and feet. The nurse assesses hydration status, as the child is refusing to eat or drink due to oral pain. Symptom management includes antipyretics for fever and analgesics for oral discomfort. The nurse educates the parents on maintaining hydration, practicing proper hygiene, and avoiding close contact with others until the symptoms resolve to prevent the spread of this viral infection.
Example 4. Chickenpox (Varicella)
A 5-year-old child presents with an itchy, vesicular rash starting on the trunk and spreading to the face and extremities. The nurse implements airborne and contact precautions to prevent transmission and educates the family about avoiding scratching to prevent secondary bacterial infections. Symptom relief includes administering antihistamines for itching and acetaminophen for fever. The parents are advised to keep the child isolated until all lesions have crusted over and are educated on the importance of the varicella vaccine for younger siblings.
Example 5. Scarlet Fever
A 7-year-old child complains of a sore throat, fever, and a rough, sandpaper-like rash. Examination reveals a “strawberry tongue” and swollen cervical lymph nodes. The nurse collects a throat swab for a rapid strep test, and a positive result confirms scarlet fever caused by Group A Streptococcus. Antibiotics (e.g., penicillin) are initiated, and the nurse educates the parents on completing the full course of antibiotics, managing fever, and maintaining hydration. Infection prevention measures, such as hand hygiene and avoiding close contact, are emphasized to prevent spreading the infection.
Practice Questions
Question 1
A 6-month-old infant diagnosed with pertussis is admitted to the hospital. Which intervention is the nurse’s priority?
A. Administer azithromycin as prescribed.
B. Provide oxygen therapy as needed.
C. Implement droplet precautions.
D. Monitor for signs of apnea.
Answer: D. Monitor for signs of apnea.
Explanation: While all the interventions are essential for managing pertussis, monitoring for apnea is the priority due to the high risk of life-threatening respiratory arrest in infants. A (administering azithromycin) addresses the infection, B (providing oxygen) supports breathing, and C (droplet precautions) prevents transmission, but none directly address the most immediate threat—apnea. NCLEX questions often prioritize life-threatening complications, following the ABCs (Airway, Breathing, Circulation) framework.
Question 2
A 4-year-old presents with a fever, sore throat, and a fine, sandpaper-like rash. The rapid strep test is positive for Group A Streptococcus. What is the nurse’s most appropriate action?
A. Administer acetaminophen for fever relief.
B. Initiate droplet precautions and start antibiotics as prescribed.
C. Advise the family to isolate the child for 2 weeks.
D. Encourage the child to drink fluids and eat solid foods.
Answer: B. Initiate droplet precautions and start antibiotics as prescribed.
Explanation: Scarlet fever is caused by Group A Streptococcus and requires antibiotic treatment to prevent complications like rheumatic fever. Droplet precautions reduce transmission risk. While A (acetaminophen) and D (hydration) are supportive interventions, they do not address the primary infection. C is incorrect because isolation is typically recommended until 24 hours after initiating antibiotics, not for two weeks.
Question 3
A 5-year-old child with chickenpox is at home and develops signs of a secondary bacterial infection. Which finding should the nurse advise the parents to report immediately?
A. Crusting of the chickenpox lesions.
B. Persistent fever of 38°C (100.4°F).
C. Pus or redness surrounding a lesion.
D. Itching and irritability.
Answer: C. Pus or redness surrounding a lesion.
Explanation: Pus or redness around a lesion indicates a secondary bacterial infection, which requires prompt medical evaluation and treatment to prevent systemic complications. A (crusting lesions) is a normal part of chickenpox healing. B (low-grade fever) and D (itching) are common symptoms of chickenpox but do not require immediate intervention. Recognizing complications is critical in NCLEX scenarios.