The integumentary system, comprising the skin, hair, nails, and glands, is the body’s largest organ system and serves as the first line of defense against external threats. It plays a critical role in protection, thermoregulation, sensation, and fluid balance. This system also participates in immune response and vitamin D synthesis. Conditions affecting the integumentary system, such as burns, pressure injuries, infections, and skin cancers, require careful assessment and management. Understanding these disorders and their nursing interventions is essential for optimal patient care and success on the NCLEX-RN®.
In studying “Integumentary” for the NCLEX-RN® exam, you should learn to assess and manage common integumentary conditions, including pressure injuries, burns, and cellulitis. Understand the principles of wound healing, infection prevention, and skin integrity maintenance. Evaluate the pathophysiology and nursing interventions for skin disorders like psoriasis, eczema, and skin cancer. Analyze strategies for promoting patient education on hygiene, sun protection, and early detection of skin changes. Additionally, apply your knowledge to prioritize care, interpret assessment findings, and develop effective nursing plans for integumentary health in clinical scenarios commonly featured in NCLEX practice questions.
Introduction of Integumentary
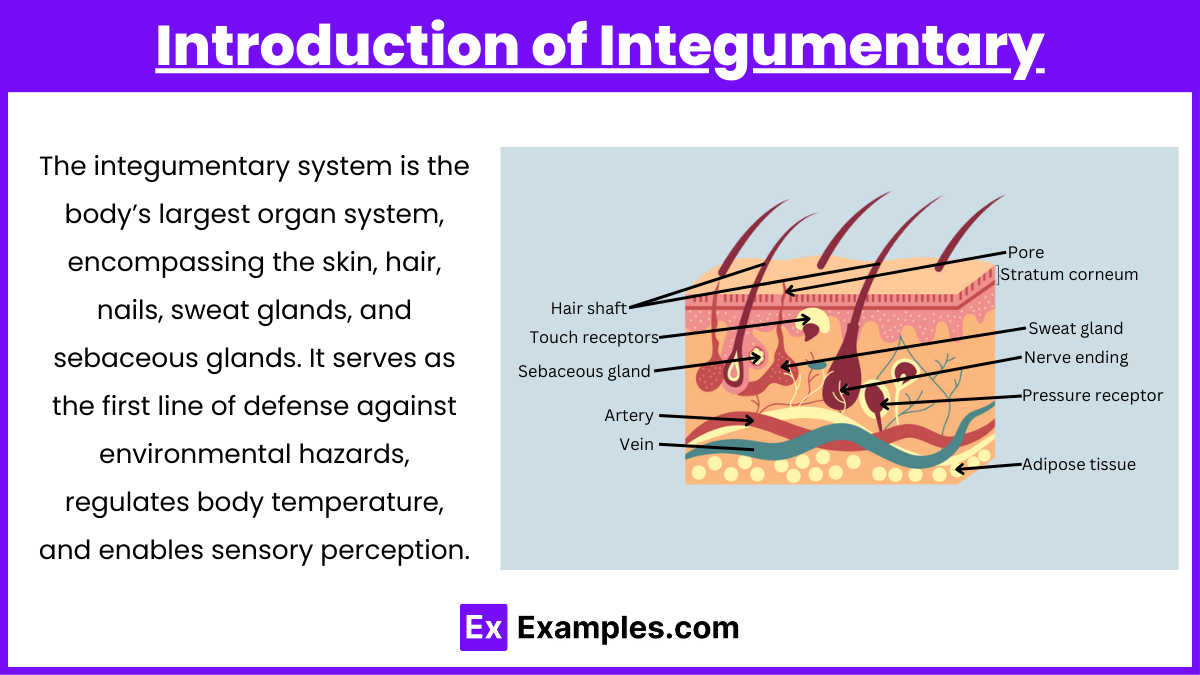
The integumentary system is the body’s largest organ system, encompassing the skin, hair, nails, sweat glands, and sebaceous glands. It serves as the first line of defense against environmental hazards, regulates body temperature, and enables sensory perception. The skin, composed of the epidermis, dermis, and subcutaneous layers, plays a critical role in protection, hydration, and vitamin D synthesis. Understanding this system is essential for recognizing and treating conditions that affect the body’s outermost structures.
The integumentary system, comprising the skin, hair, nails, and glands, is essential for protection, sensation, and thermoregulation. For the NCLEX-RN® exam, it is crucial to understand common disorders, clinical manifestations, nursing interventions, and patient education related to this system.
Common Integumentary Disorders
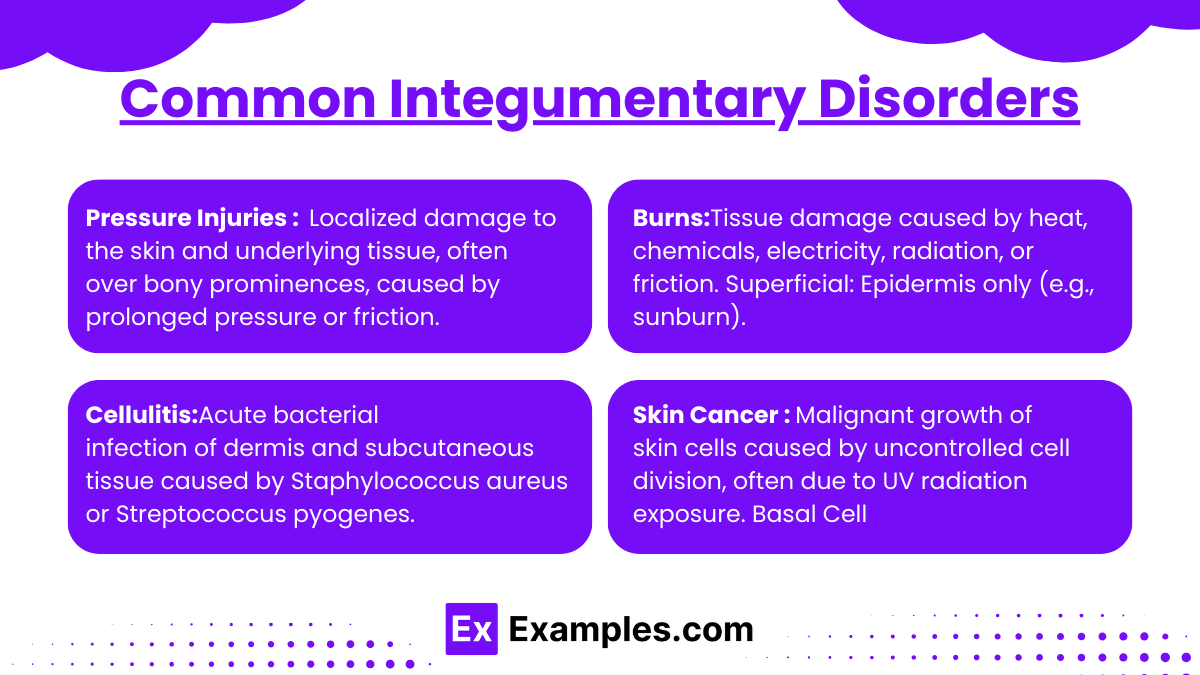
- Pressure Injuries : Localized damage to the skin and underlying tissue, often over bony prominences, caused by prolonged pressure or friction.
- Stages:
- Stage I: Non-blanchable erythema.
- Stage II: Partial-thickness skin loss.
- Stage III: Full-thickness loss with possible adipose tissue exposure.
- Stage IV: Full-thickness with exposed bone, muscle, or tendon.
- Interventions:
- Reposition every 2 hours, use pressure-relieving devices, and ensure adequate nutrition.
- Assess skin regularly for early signs of breakdown.
- Stages:
- Burns:Tissue damage caused by heat, chemicals, electricity, radiation, or friction.
- Classification:
- Superficial: Epidermis only (e.g., sunburn).
- Partial Thickness: Epidermis and part of the dermis.
- Full Thickness: Extends into subcutaneous tissue or deeper.
- Interventions:
- Fluid resuscitation (Parkland formula for burns), pain management, wound care, and infection prevention.
- Classification:
- Cellulitis:Acute bacterial infection of the dermis and subcutaneous tissues, commonly caused by Staphylococcus aureus or Streptococcus pyogenes.
- Causes: Bacterial infection (Staphylococcus, Streptococcus).
- Symptoms: Red, swollen, painful area, warmth, fever.
- Interventions: Antibiotics, elevate affected limb, monitor for sepsis.
- Skin Cancer : Malignant growth of skin cells caused by uncontrolled cell division, often due to UV radiation exposure.
- Types:
- Basal Cell Carcinoma (BCC): Most common, rarely metastasizes.
- Squamous Cell Carcinoma (SCC): Potential for metastasis.
- Malignant Melanoma: High metastatic potential; evaluate using the ABCDE rule:
- A: Asymmetry
- B: Border irregularity
- C: Color variation
- D: Diameter >6mm
- E: Evolution or change in appearance.
Nursing Interventions for Integumentary Disorders
- Assessment:
- Inspect and palpate for color, moisture, texture, turgor, lesions, and ulcers.
- Document size, depth, and exudate in wounds.
- Hygiene and Skin Care:
- Use mild cleansers and avoid irritants.
- Keep skin hydrated to maintain integrity.
- Infection Control:
- Maintain aseptic techniques during wound care.
- Educate on hand hygiene and recognizing signs of infection.
- Education:
- Teach self-care for chronic conditions (e.g., psoriasis, eczema).
- Stress sun protection and proper wound care.
Examples
Example 1: Pressure Injuries and Nursing Interventions
A bedridden patient is admitted with a Stage II pressure injury on their sacrum. The nurse is asked to develop a care plan to promote healing and prevent further damage. The correct nursing actions include repositioning the patient every two hours, maintaining a clean and dry wound environment, and providing a high-protein, calorie-dense diet to promote tissue repair. NCLEX-style questions may ask the nurse to prioritize these actions or recognize signs of worsening injury.
Example 2: Burn Management and Fluid Resuscitation
A 40-year-old patient with partial-thickness burns over 30% of their body surface area is brought to the emergency department. The nurse calculates the fluid resuscitation needs using the Parkland formula and ensures the patient receives the appropriate volume of lactated Ringer’s solution within the first 24 hours. NCLEX questions may require the nurse to prioritize airway management, assess signs of fluid overload, or recognize infection in burn wounds.
Example 3: Skin Cancer Detection and Patient Education
A patient presents with a lesion on their arm that has changed in size, has irregular borders, and varies in color. The nurse assesses the lesion using the ABCDE criteria for melanoma. The nurse educates the patient on the importance of avoiding sun exposure, using sunscreen with SPF 30 or higher, and performing regular self-skin checks. NCLEX questions may focus on identifying risk factors for skin cancer or recognizing abnormal lesions.
Example 4: Shingles (Herpes Zoster) and Pain Management
An elderly patient with a history of chickenpox presents with a painful, blistering rash along a dermatomal pattern on their back. The nurse administers prescribed antiviral medication (e.g., acyclovir) and educates the patient on keeping the affected area clean and dry. Questions may test the nurse’s ability to recognize complications like postherpetic neuralgia or the effectiveness of antiviral therapy in reducing symptom severity.
Example 5: Cellulitis Diagnosis and Treatment
A patient comes to the clinic with redness, warmth, swelling, and tenderness on their lower leg. The nurse suspects cellulitis and prepares the patient for blood tests and wound cultures to identify the causative organism. The nurse administers the prescribed antibiotics and educates the patient on the importance of completing the full antibiotic course. NCLEX questions may involve identifying systemic signs of sepsis, educating the patient about elevating the affected limb, or recognizing the effectiveness of treatment.
Practice Questions
Question 1
A patient with iron deficiency anemia is prescribed ferrous sulfate. Which instruction should the nurse include in the teaching plan?
A. Take the medication with milk to improve absorption.
B. Take the medication on an empty stomach if tolerated.
C. Avoid foods high in vitamin C when taking the medication.
D. Expect stools to remain unchanged in color while on therapy.
Answer: B. Take the medication on an empty stomach if tolerated.
Explanation:
- Ferrous sulfate is best absorbed on an empty stomach, as food can interfere with its absorption. However, if gastrointestinal upset occurs, it may be taken with a small amount of food.
- Option A: Milk and dairy products decrease iron absorption due to the calcium content.
- Option C: Vitamin C enhances the absorption of iron and should not be avoided.
- Option D: Iron supplements commonly cause dark, tarry stools as a normal side effect, so this statement is incorrect.
Question 2
A patient receiving chemotherapy for breast cancer reports fatigue and shortness of breath. Which laboratory finding is most consistent with these symptoms?
A. Hemoglobin 8.2 g/dL
B. Platelet count 150,000/μL
C. White blood cell (WBC) count 5,000/μL
D. Serum potassium 4.0 mEq/L
Answer: A. Hemoglobin 8.2 g/dL
Explanation:
- Option A: A hemoglobin level of 8.2 g/dL indicates anemia, a common side effect of chemotherapy, leading to fatigue and shortness of breath due to decreased oxygen-carrying capacity.
- Option B: The platelet count is within normal limits (150,000–450,000/μL) and does not explain the symptoms.
- Option C: The WBC count is also within normal limits (4,500–11,000/μL) and does not relate to the symptoms.
- Option D: A potassium level of 4.0 mEq/L is normal (3.5–5.0 mEq/L) and not associated with fatigue or shortness of breath.
Question 3
The nurse is caring for a patient with acute leukemia undergoing chemotherapy. Which of the following is the most important intervention to prevent complications?
A. Monitor the patient for signs of bleeding.
B. Assess for signs of infection.
C. Encourage high-impact exercise.
D. Administer antiemetic medication as prescribed.
Answer: B. Assess for signs of infection.
Explanation:
- Option B: Patients with acute leukemia are immunocompromised due to the disease and chemotherapy, placing them at high risk for infections. Monitoring for fever, increased WBC counts, or localized signs of infection is critical.
- Option A: Although bleeding risks exist (due to thrombocytopenia), preventing infection is a higher priority because infections can rapidly become life-threatening.
- Option C: High-impact exercise is not recommended during active treatment as patients are often fatigued or at risk for injury.
- Option D: Administering antiemetics helps manage nausea but does not address the most critical complication, which is infection.