The integumentary system plays a vital role in maintaining a child’s health by protecting against infection, regulating temperature, and preventing dehydration. In pediatric care, the skin is more delicate and susceptible to conditions such as eczema, impetigo, burns, and diaper dermatitis. Effective management requires prompt assessment, interventions to prevent complications, and education for caregivers. For the NCLEX-RN®, understanding the unique characteristics of children’s skin and prioritizing care for conditions like infections or burns is essential to ensure safety and promote optimal healing outcomes.
Learning Objectives
In studying “Child Health: Integumentary” for the NCLEX-RN® exam, you should learn to understand the unique characteristics of pediatric skin and common conditions such as eczema, impetigo, and burns. Analyze the principles of assessment, prevention, and management of integumentary disorders in children, focusing on prioritizing care and recognizing complications like infection and dehydration. Evaluate evidence-based interventions, including medication administration, wound care, and family education. Additionally, explore the role of the nurse in promoting hygiene, managing symptoms, and preventing disease progression. Apply this knowledge to interpret pediatric skin-related scenarios in practice questions, emphasizing critical thinking and safe, effective care.
Key Concepts of Integumentary
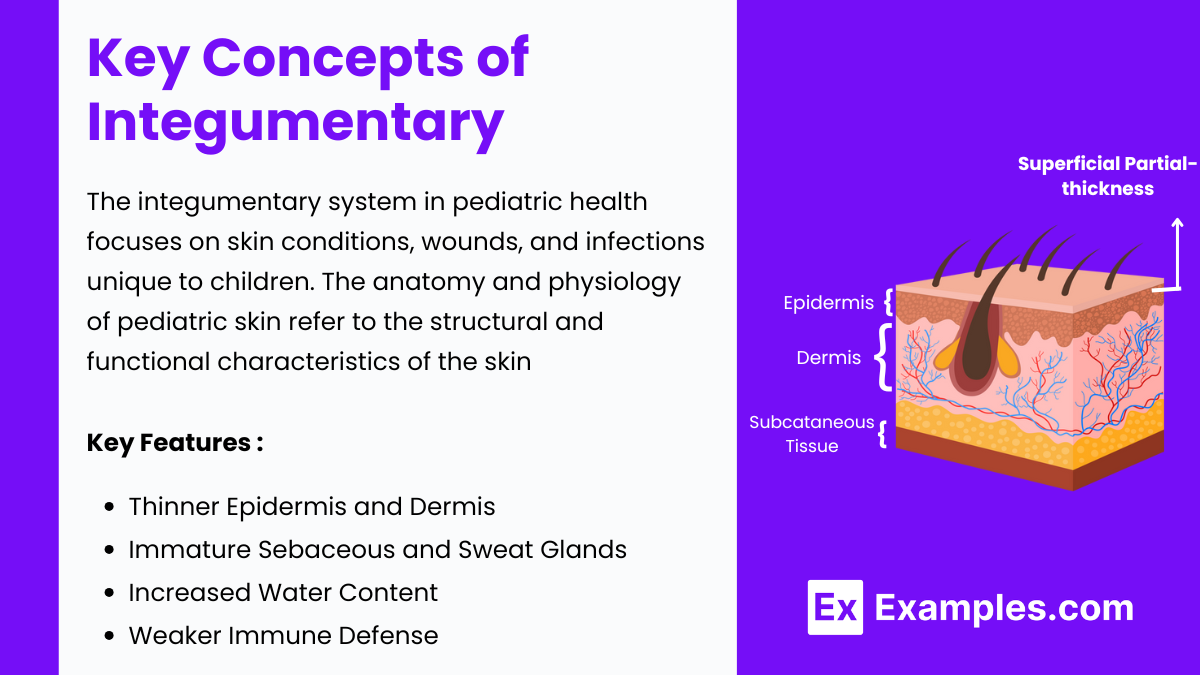
The integumentary system in pediatric health focuses on skin conditions, wounds, and infections unique to children. Mastering this topic is essential for success on the NCLEX-RN® exam as it evaluates your ability to prioritize care, recognize critical conditions, and educate families effectively. The anatomy and physiology of pediatric skin refer to the structural and functional characteristics of the skin in infants and children, which differ significantly from adult skin due to its immaturity and developmental state. Pediatric skin is thinner, more permeable, and less able to regulate temperature and moisture, making it more susceptible to injuries, infections, and irritations.
Key features:
- Thinner Epidermis and Dermis: Leads to increased risk of trauma and enhanced absorption of topical agents.
- Immature Sebaceous and Sweat Glands: Results in reduced oil production and inefficient thermoregulation.
- Increased Water Content: Contributes to faster dehydration and altered healing processes.
- Weaker Immune Defense: Heightens susceptibility to infections due to underdeveloped skin barrier and immune response.
Common Pediatric Integumentary Conditions
1. Eczema (Atopic Dermatitis)
Eczema, also known as Atopic Dermatitis, is a chronic inflammatory skin condition that often begins in childhood and may persist into adulthood. Characterized by periods of flare-ups and remission, eczema causes the skin to become red, itchy, and inflamed. While the exact cause remains unknown, it is believed to result from a combination of genetic, environmental, and immune system factors.
- Characteristics: Chronic, itchy rash with dry, scaly skin. Often seen in flexor areas (elbows, knees).
- Triggers: Allergens, irritants, stress, temperature changes.
- Nursing Management:
- Apply moisturizers (e.g., petroleum-based or ceramide creams).
- Use anti-inflammatory medications (e.g., corticosteroid creams).
- Educate parents on avoiding triggers and scratching.
2. Impetigo
Impetigo is a highly contagious bacterial skin infection that primarily affects children but can occur in individuals of any age. It is characterized by red sores or blisters that rupture, ooze fluid, and form a yellowish-brown crust. The infection is commonly caused by Staphylococcus aureus or Streptococcus pyogenes bacteria and is typically spread through direct contact with an infected person or contaminated surfaces.
- Cause: Bacterial infection (Staphylococcus aureus or Streptococcus pyogenes).
- Characteristics: Honey-colored crusted lesions, often around the mouth and nose.
- Nursing Management:
- Encourage proper hand hygiene.
- Administer topical antibiotics (e.g., mupirocin) or systemic antibiotics for severe cases.
- Educate parents about contagion precautions.
3. Diaper Dermatitis
Diaper dermatitis, commonly known as diaper rash, is a form of irritant contact dermatitis that occurs in the diaper area of infants and young children. It is characterized by inflammation, redness, and irritation of the skin caused by prolonged exposure to moisture, friction, and irritants such as urine, feces, or harsh diaper materials. This condition may also be exacerbated by secondary infections, such as yeast or bacteria, and typically manifests as a red, patchy rash in areas covered by a diaper. Early treatment and preventive measures are essential to reduce discomfort and promote healing.
- Cause: Prolonged exposure to irritants like urine or feces.
- Characteristics: Red, inflamed rash in diaper area; may develop secondary yeast infection.
- Nursing Management:
- Use barrier creams (e.g., zinc oxide).
- Keep diaper area clean and dry.
- Recommend frequent diaper changes.
Nursing Priorities
1.Assessment
- Inspect the skin for color changes, lesions, texture, and hydration.
- Monitor for systemic signs of infection (e.g., fever).
2.Interventions
- Prioritize infection control measures.
- Administer appropriate medications and monitor for side effects.
- Educate parents about preventive measures and proper skincare.
3.Education
- Teach caregivers about early recognition of skin conditions.
- Stress the importance of hygiene and avoiding allergens.
Examples
Example 1. Eczema (Atopic Dermatitis)
A child presents with red, scaly, and itchy skin in the flexural areas such as elbows and knees. The condition often worsens during dry weather or exposure to allergens. Nurses should prioritize teaching parents about moisturizing the child’s skin frequently, applying topical corticosteroids as prescribed, and identifying triggers like certain soaps, fabrics, or foods. Education on avoiding scratching is crucial to prevent secondary infections.
Example 2. Impetigo
A 4-year-old child has multiple honey-colored crusted lesions around their mouth and nose. The nurse identifies this as impetigo, a highly contagious bacterial skin infection. Interventions include applying topical antibiotics (e.g., mupirocin) and instructing caregivers to maintain strict hygiene, including washing hands and disinfecting shared items. The family should be informed about preventing the spread by keeping the child away from daycare or school until the infection clears.
Example 3. Diaper Dermatitis
A 9-month-old infant presents with redness and irritation in the diaper area, with possible satellite lesions indicating a secondary yeast infection. The nurse advises frequent diaper changes, cleansing the area with warm water and mild soap, and applying a thick barrier cream like zinc oxide. If a fungal infection is suspected, antifungal ointments like nystatin may be prescribed. Education focuses on preventing prolonged exposure to moisture and irritants.
Example 4. Burn Management
A toddler sustains partial-thickness burns on their arm after touching a hot surface. The nurse assesses the burn’s depth, size, and location and monitors for signs of dehydration or infection. Immediate interventions include pain management, applying sterile dressings, and ensuring proper hydration. Parents are educated on wound care, recognizing infection signs, and preventing further incidents by childproofing their home environment.
Example 5. Tinea Capitis
A 7-year-old child presents with round, scaly patches of hair loss on the scalp. The nurse recognizes this as tinea capitis, a fungal infection requiring systemic antifungal therapy, such as oral griseofulvin. Topical treatments alone are ineffective for scalp infections. The nurse provides education on maintaining hygiene, avoiding sharing personal items like combs, and completing the entire course of medication to prevent recurrence.
Practice Questions
Question 1
A 6-month-old infant presents with erythematous patches in the diaper area with satellite lesions. The nurse suspects diaper dermatitis complicated by a yeast infection. What is the most appropriate nursing intervention?
A. Apply a zinc oxide barrier cream.
B. Clean the area with alcohol-based wipes and keep it open to air.
C. Apply an antifungal cream to the affected area.
D. Increase fluid intake to promote hydration.
Answer: C. Apply an antifungal cream to the affected area.
Explanation: Satellite lesions are a hallmark of Candida albicans infection, requiring antifungal treatment such as nystatin or clotrimazole.
- A Zinc oxide is suitable for simple irritant diaper dermatitis but ineffective for fungal infections.
- B Alcohol-based wipes can irritate the skin further and are not recommended for sensitive areas.
- D Increased hydration is helpful for overall health but does not directly treat the infection.
Question 2
A school-aged child has honey-colored crusted lesions around their mouth and nose. Which action should the nurse prioritize?
A. Clean the lesions with warm water and apply petroleum jelly.
B. Initiate contact precautions and administer topical antibiotics.
C. Administer oral antihistamines to relieve itching.
D. Apply a corticosteroid cream to reduce inflammation.
Answer: B. Initiate contact precautions and administer topical antibiotics.
Explanation: Honey-colored crusted lesions are indicative of impetigo, a contagious bacterial infection caused by Staphylococcus aureus or Streptococcus pyogenes. Contact precautions prevent spread, and topical antibiotics (e.g., mupirocin) are the treatment of choice.
- A Cleaning the lesions is helpful but does not address the infection. Petroleum jelly does not treat the bacteria.
- C Antihistamines may alleviate itching but are not a primary treatment.
- D Corticosteroids are not indicated for bacterial infections and can worsen the condition.
Question 3
A toddler with atopic dermatitis has dry, scaly patches on the flexor surfaces of the arms and legs. What teaching should the nurse provide to the parents?
A. Use fragrance-free moisturizers and apply immediately after bathing.
B. Bathe the child with hot water to open the pores and reduce dryness.
C. Apply over-the-counter hydrocortisone cream daily for prevention.
D. Wash the affected areas with antibacterial soap to prevent infection.
Answer: A. Use fragrance-free moisturizers and apply immediately after bathing.
Explanation: Fragrance-free moisturizers applied immediately after bathing help retain skin moisture and reduce dryness, which is key to managing atopic dermatitis.
- B Hot water can dry out the skin further, worsening symptoms.
- C Hydrocortisone should only be used as prescribed for flare-ups, not daily prevention.
- D Antibacterial soap can irritate the sensitive skin of children with eczema.