Labor and delivery are critical processes in maternal and newborn health, encompassing the stages of childbirth from the onset of contractions to postpartum recovery. For the NCLEX-RN®, understanding these stages, including cervical dilation, fetal descent, and placental delivery, is essential. Key nursing responsibilities include monitoring fetal heart rate, managing maternal pain, and intervening during complications like dystocia or fetal distress. Mastery of labor/delivery ensures safe and effective nursing care, emphasizing maternal well-being and newborn health while prioritizing timely interventions to prevent adverse outcomes.
Learning Objectives
In studying "Maternal & Newborn Health: Labor/Delivery" for the NCLEX-RN®, you should learn to understand the physiological stages of labor, including cervical dilation, fetal descent, and placental delivery. Analyze nursing interventions such as fetal heart monitoring, pain management, and management of complications like dystocia and postpartum hemorrhage. Evaluate the principles of newborn care immediately after delivery, including APGAR scoring, thermal regulation, and respiratory support. Additionally, explore the role of evidence-based practices in promoting maternal and fetal well-being and apply your understanding to interpret scenarios and prioritize nursing interventions effectively in NCLEX-style practice questions.
Stages of Labor
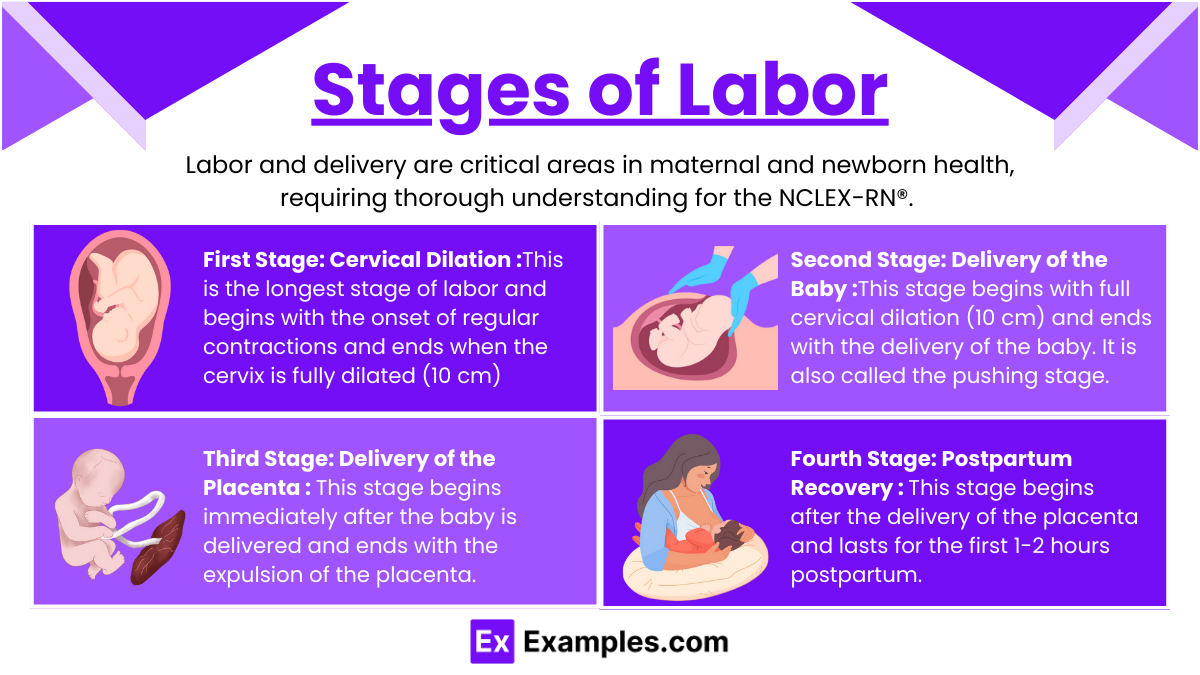
Labor and delivery are critical areas in maternal and newborn health, requiring thorough understanding for the NCLEX-RN®. This topic covers physiological processes, nursing interventions, complications, and newborn care during labor and delivery. Mastery of this section ensures your ability to provide safe and effective nursing care to mothers and newborns. Labor is divided into four stages, each with distinct characteristics:
First Stage: Cervical Dilation : This is the longest stage of labor and begins with the onset of regular contractions and ends when the cervix is fully dilated (10 cm). It is further divided into three phases: latent, active, and transition.
Latent Phase: Cervix dilates 0-3 cm; mild contractions.
Active Phase: Cervix dilates 4-7 cm; moderate to strong contractions.
Transition Phase: Cervix dilates 8-10 cm; strong, frequent contractions.
Nursing Care:
Monitor fetal heart rate (FHR) and maternal vital signs.
Encourage relaxation and breathing techniques.
Administer pain management as per protocol.
Second Stage: Delivery of the Baby : This stage begins with full cervical dilation (10 cm) and ends with the delivery of the baby. It is also called the pushing stage.
Begins with full cervical dilation and ends with delivery.
Nursing Care:
Support effective pushing techniques.
Monitor FHR and ensure sterile field.
Provide perineal support to prevent tearing.
Third Stage: Delivery of the Placenta : This stage begins immediately after the baby is delivered and ends with the expulsion of the placenta.
Usually lasts 5-30 minutes after the baby is delivered.
Nursing Care:
Observe for signs of placental separation.
Monitor for excessive bleeding.
Administer uterotonics (e.g., oxytocin) as prescribed.
Fourth Stage: Postpartum Recovery : This stage begins after the delivery of the placenta and lasts for the first 1-2 hours postpartum. It focuses on maternal recovery and monitoring for complications.
First 1-2 hours post-delivery.
Nursing Care:
Monitor maternal vital signs, lochia, and uterine firmness.
Encourage bonding and breastfeeding.
Assess for complications like hemorrhage or infection.
Maternal Assessment During Labor
Fetal Monitoring:
Evaluate baseline FHR (110-160 bpm).
Assess variability, accelerations, and decelerations.
Respond to abnormalities (e.g., repositioning, oxygen, amnioinfusion).
Contraction Patterns:
Measure frequency, duration, and intensity.
Ensure adequate rest between contractions.
Maternal Vital Signs:
Monitor blood pressure, pulse, and temperature for signs of distress.
Cervical Exams:
Assess dilation, effacement, and station.
Complications and Interventions
Precipitous Labor:
Labor lasting less than 3 hours.
Interventions: Ensure a safe, controlled environment; prepare for rapid delivery.
Dystocia (Difficult Labor):
Causes include uterine dysfunction, fetal malpresentation.
Interventions: Administer oxytocin, assist with repositioning, or prepare for cesarean.
Fetal Distress:
Signs: Persistent late decelerations, absent variability.
Interventions: Reposition mother, administer oxygen, and consider emergent delivery.
Prolapsed Umbilical Cord:
Cord precedes the fetus, compressing blood flow.
Interventions: Elevate presenting part, place in knee-chest position, and prepare for emergency cesarean.
Postpartum Hemorrhage:
Excessive bleeding after delivery.
Interventions: Massage uterus, administer uterotonics, and assess for retained placental fragments.
Newborn Care Immediately After Birth
APGAR Scoring (1 and 5 minutes post-birth): The APGAR score is an objective method to assess the newborn's immediate physical condition and need for resuscitation. The score is given at 1 and 5 minutes after birth.
Appearance (Skin color): Pink body with pink extremities (2 points); pink body with blue extremities (1 point); pale or blue all over (0 points).
Pulse (Heart rate): Greater than 100 bpm (2 points); less than 100 bpm (1 point); absent (0 points).
Grimace (Reflex irritability): Cries or pulls away when stimulated (2 points); weak response (1 point); no response (0 points).
Activity (Muscle tone): Active motion (2 points); some flexion (1 point); limp (0 points).
Respiration (Breathing effort): Strong cry (2 points); weak cry or slow breathing (1 point); absent breathing (0 points).
Intervention required if score ≤6.
Thermal Regulation: Newborns are prone to heat loss due to their large surface area, thin skin, and limited fat reserves. Maintaining a warm environment is essential.
Steps to Ensure Warmth:
Dry the Newborn Immediately: Use a warm, soft towel to dry the baby to prevent evaporative heat loss.
Skin-to-Skin Contact: Place the baby on the mother’s bare chest; this promotes bonding and maintains body temperature.
Use a Radiant Warmer: If skin-to-skin contact is not possible, place the newborn under a radiant warmer.
Warm Blankets: Wrap the baby in pre-warmed blankets, ensuring the head is covered with a cap to prevent heat loss from the head.
Monitor for signs of hypothermia.
Respiratory Support: Establishing effective breathing is a priority for newborns immediately after birth.
Clear airway using suction if needed.
Stimulate crying to promote lung expansion.
Cord Clamping and Care: The umbilical cord must be clamped and cut to prevent bleeding and infection.
Timing of Cord Clamping:
Delayed clamping (1-3 minutes): Recommended as it increases blood volume and iron stores in the newborn.
Immediate clamping is done in emergencies where the newborn requires resuscitation.
Cord Care:
Apply a sterile clamp approximately 2-3 cm from the baby’s abdomen.
Cut the cord using sterile scissors.
Keep the cord stump clean and dry to prevent infection.
Examples
Example 1: Fetal Heart Rate (FHR) Monitoring and Intervention
A mother in active labor shows repetitive late decelerations on the fetal heart monitor. Late decelerations indicate uteroplacental insufficiency and potential fetal distress. The nurse must implement immediate interventions such as repositioning the mother to a left-lateral position, administering oxygen via a non-rebreather mask, and increasing IV fluid administration to enhance placental perfusion. If no improvement occurs, notify the healthcare provider and prepare for possible emergency cesarean delivery. Understanding how to prioritize care during fetal distress is critical for the NCLEX-RN®.
Example 2: Precipitous Labor Management
A woman arrives in the labor and delivery unit in advanced labor, with contractions every 2 minutes and strong intensity. On assessment, the cervix is fully dilated, and the baby’s head is crowning. The nurse prepares for immediate delivery by creating a sterile field, supporting the perineum to prevent tearing, and guiding the mother to push effectively. After delivery, the nurse clamps and cuts the umbilical cord and monitors the mother for postpartum hemorrhage. Precipitous labor scenarios test the nurse's ability to manage urgent situations with speed and precision.
Example 3: Shoulder Dystocia Intervention
During the second stage of labor, the baby's head delivers, but the shoulders become impacted behind the mother's pubic bone. The nurse applies the McRoberts maneuver (flexing the mother’s legs tightly against her abdomen) and applies suprapubic pressure to dislodge the shoulder. Avoid fundal pressure, as it can worsen the situation. If maneuvers fail, the provider may perform additional techniques to deliver the baby. This scenario demonstrates the importance of recognizing obstetric emergencies and implementing evidence-based interventions.
Example 4: Postpartum Hemorrhage Management
After a normal vaginal delivery, the mother experiences heavy vaginal bleeding and passes large clots. On assessment, the uterus is soft and boggy, indicating uterine atony. The nurse immediately performs fundal massage to promote uterine contraction, administers prescribed uterotonics like oxytocin or methylergonovine, and monitors vital signs closely. If bleeding persists, the nurse prepares the patient for additional interventions, such as intrauterine tamponade or surgical management. This case emphasizes the nurse’s role in identifying and managing life-threatening postpartum complications.
Example 5: Neonatal Resuscitation
A newborn delivered at 39 weeks gestation has an APGAR score of 4 at one minute due to poor respiratory effort and bradycardia. The nurse initiates neonatal resuscitation by drying and stimulating the baby, suctioning the airway, and providing positive pressure ventilation with a bag-mask device. Heart rate and oxygen saturation are monitored continuously. If the heart rate remains below 60 bpm, chest compressions are started. This example focuses on critical thinking and rapid response to stabilize a compromised newborn, aligning with NCLEX-RN® priorities.
Practice Questions
Question 1
A laboring client is in the second stage of labor. The fetal heart rate is consistently 100 bpm, and late decelerations are noted. What is the nurse's priority action?
A. Reposition the client to a left lateral position.
B. Administer oxygen via face mask.
C. Notify the healthcare provider immediately.
D. Increase the IV oxytocin infusion rate.
Answer: A. Reposition the client to a left lateral position.
Explanation:
Repositioning (A) helps improve uteroplacental blood flow, which can alleviate fetal hypoxia and reduce late decelerations.
Administering oxygen (B) is important but should follow repositioning. Oxygen improves fetal oxygenation once blood flow is optimized.
Notifying the healthcare provider (C) is necessary, but immediate nursing interventions should be prioritized first.
Increasing the oxytocin rate (D) is contraindicated in the presence of fetal distress, as it can exacerbate hypoxia by intensifying contractions.
Question 2
A nurse is monitoring a laboring client who is 6 cm dilated and 100% effaced. The client reports severe back pain with each contraction. Which action is most effective in relieving the client’s discomfort?
A. Encourage the client to use breathing techniques.
B. Perform sacral counterpressure during contractions.
C. Reposition the client to a semi-Fowler's position.
D. Administer prescribed IV pain medication.
Answer: B. Perform sacral counterpressure during contractions.
Explanation:
Sacral counterpressure (B) is highly effective for managing back pain caused by fetal occiput posterior (OP) positioning. It alleviates pressure on the sacrum during contractions.
Breathing techniques (A) can help with overall pain management but are less specific to back pain relief.
Semi-Fowler's position (C) does not address the specific discomfort of back labor. Instead, positions like hands-and-knees may help rotate the fetus and relieve pain.
Administering IV pain medication (D) can be an option, but non-pharmacologic methods should be attempted first.
Question 3
During the third stage of labor, the nurse observes the umbilical cord lengthening and a gush of blood from the vagina. What is the nurse’s next action?
A. Apply fundal pressure to assist with placental expulsion.
B. Gently pull on the umbilical cord to hasten delivery of the placenta.
C. Document findings and wait for spontaneous placental expulsion.
D. Assess the uterus for firmness and massage if boggy.
Answer: C. Document findings and wait for spontaneous placental expulsion.
Explanation:
Documenting findings and waiting (C) is the correct action as these signs indicate placental separation. The placenta will typically deliver spontaneously without interference.
Applying fundal pressure (A) is not recommended as it may cause uterine inversion or trauma.
Pulling on the umbilical cord (B) can lead to uterine inversion or retained placental fragments, which are serious complications.
Uterine massage (D) is only indicated for postpartum hemorrhage or if the uterus is boggy after placental delivery.