Medication administration is a fundamental aspect of nursing practice and a crucial focus of the NCLEX-RN® exam. It involves the accurate preparation, delivery, and documentation of prescribed medications while prioritizing patient safety. Nurses must adhere to the “Five Rights” of medication administration and follow protocols to prevent errors. Mastery of dosage calculations, route selection, and understanding drug classifications is essential for success. Proficiency in medication administration ensures effective patient care, minimizes adverse drug events, and significantly enhances performance on the NCLEX-RN® exam.
Learning Objectives
In studying “Pharmacology: Medication Administration” for the NCLEX-RN® exam, you should learn to understand the principles and procedures for safe medication administration, including the “Five Rights” and “Three Checks.” Analyze the various routes of drug administration (oral, IV, IM, subcutaneous, etc.) and their impact on drug absorption, distribution, metabolism, and excretion. Evaluate dosage calculations, pediatric considerations, and prevention of medication errors. Explore techniques for handling high-alert medications, patient education, and error reporting. Apply your understanding to clinical scenarios and NCLEX-RN® practice questions, ensuring the ability to make safe, evidence-based decisions during medication administration in healthcare settings.
Principles of Safe Medication Administration
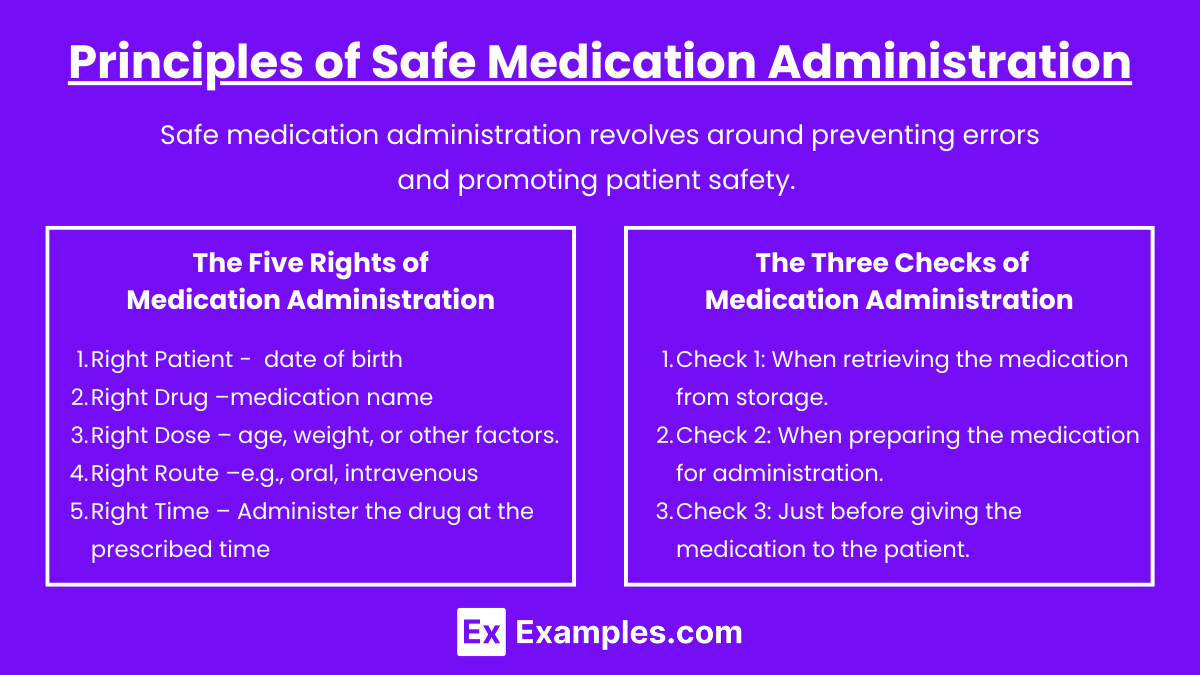
Safe medication administration revolves around preventing errors and promoting patient safety. To achieve this, nurses must adhere to specific protocols and guidelines.
The Five Rights of Medication Administration
- Right Patient – Confirm the patient’s identity using two identifiers (e.g., name and date of birth).
- Right Drug – Check that the medication name matches the prescription.
- Right Dose – Verify the correct dosage and adjust for age, weight, or other factors.
- Right Route – Ensure the medication is administered via the correct route (e.g., oral, intravenous, subcutaneous).
- Right Time – Administer the drug at the prescribed time or within an acceptable timeframe.
The Three Checks of Medication Administration
- Check 1: When retrieving the medication from storage.
- Check 2: When preparing the medication for administration.
- Check 3: Just before giving the medication to the patient.
Adhering to the Five Rights and Three Checks prevents medication errors and ensures patient safety.
Routes of Medication Administration
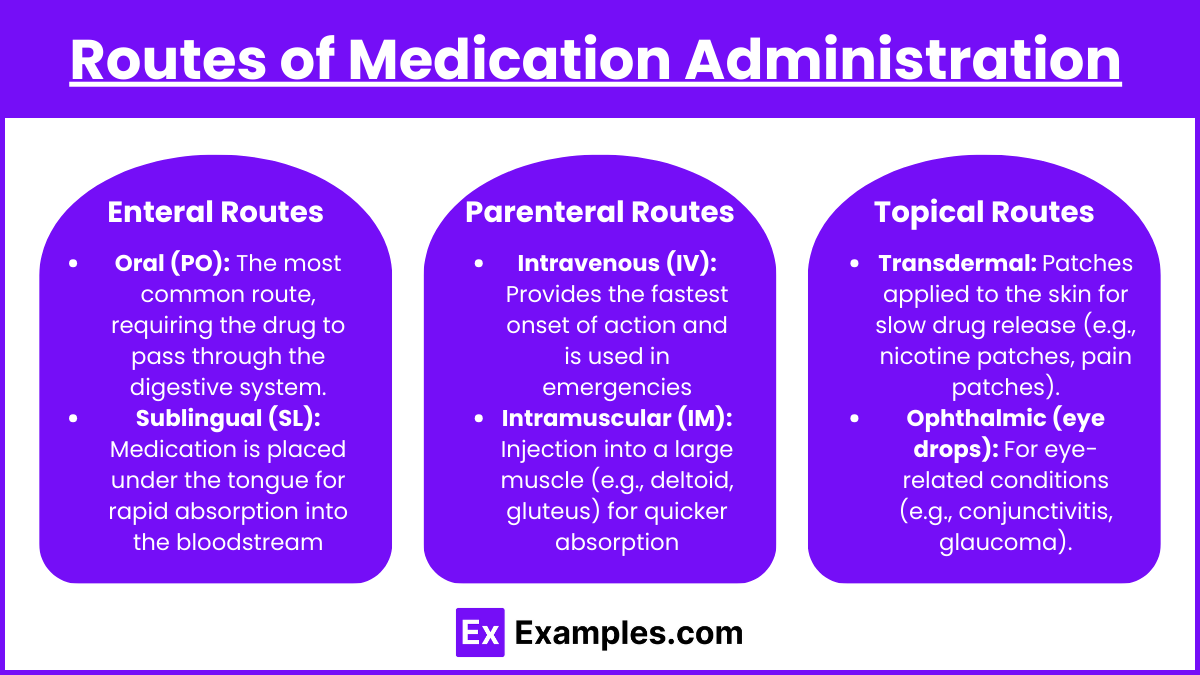
The route of administration affects drug absorption and therapeutic effect. NCLEX-RN® exam questions often ask about these routes and when to use them.
Enteral Routes
- Oral (PO): The most common route, requiring the drug to pass through the digestive system.
- Sublingual (SL): Medication is placed under the tongue for rapid absorption into the bloodstream (e.g., nitroglycerin).
- Buccal: Medication is placed between the cheek and gums, where it dissolves for local or systemic absorption.
- Rectal (PR): Used for unconscious patients or those with nausea/vomiting.
Parenteral Routes
- Intravenous (IV): Provides the fastest onset of action and is used in emergencies or for continuous infusions.
- Intramuscular (IM): Injection into a large muscle (e.g., deltoid, gluteus) for quicker absorption than subcutaneous.
- Subcutaneous (SC): Injection into fatty tissue under the skin for slower, steady drug release (e.g., insulin, heparin).
- Intradermal (ID): Used for diagnostic testing (e.g., tuberculin skin test).
Topical Routes
- Transdermal: Patches applied to the skin for slow drug release (e.g., nicotine patches, pain patches).
- Ophthalmic (eye drops): For eye-related conditions (e.g., conjunctivitis, glaucoma).
- Otic (ear drops): For local treatment of ear infections or wax removal.
- Nasal: Used for local or systemic action (e.g., decongestant nasal sprays).
The NCLEX-RN® exam may test your knowledge of when and why specific routes are used and how they affect drug absorption.
Dosage Calculations and Error Prevention
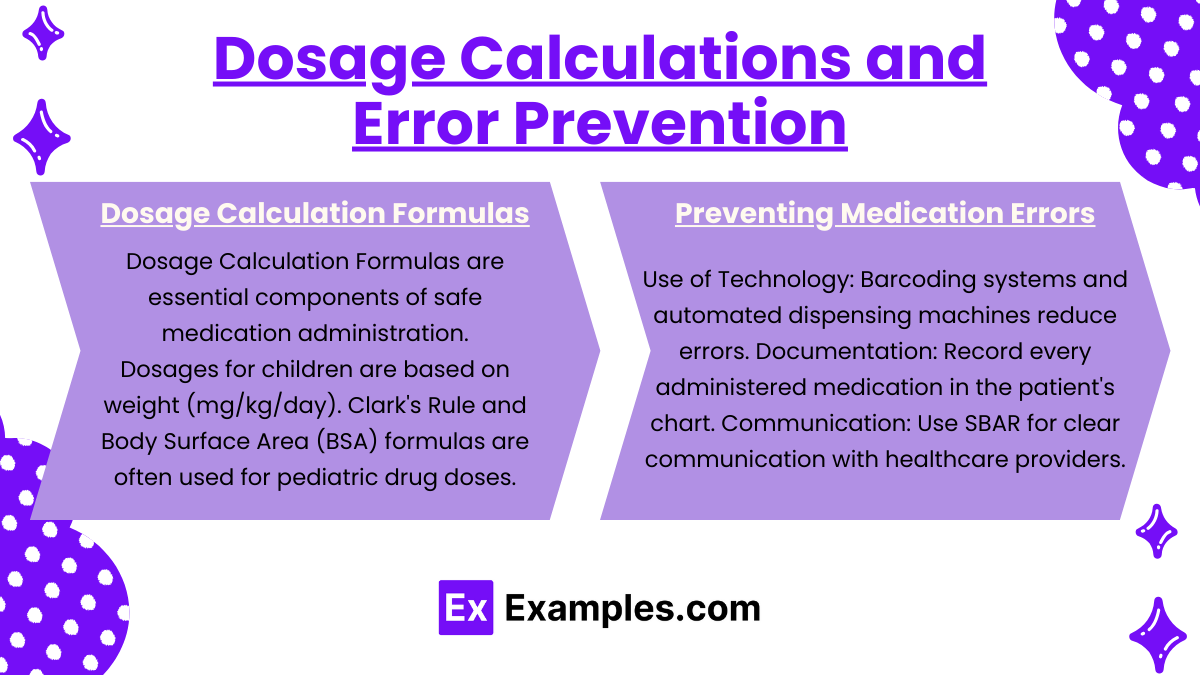
Accurate dosage calculations are essential to avoid patient harm, particularly in pediatric and critical care settings. The NCLEX-RN® exam often includes dosage calculation questions.
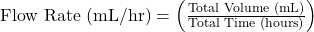
Dosage Calculation Formulas : Dosage Calculation Formulas and Preventing Medication Errors are essential components of safe medication administration for the NCLEX-RN® exam.
- Basic Formula:
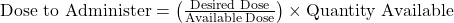
- IV Flow Rate Calculation:
- Pediatric Dosage:
- Dosages for children are based on weight (mg/kg/day).
- Clark’s Rule and Body Surface Area (BSA) formulas are often used for pediatric drug doses.
Preventing Medication Errors :
- Use of Technology: Barcoding systems and automated dispensing machines reduce errors.
- Documentation: Record every administered medication in the patient’s chart.
- Communication: Use SBAR (Situation, Background, Assessment, Recommendation) for clear communication with healthcare providers.
- Reporting Errors: If a medication error occurs, complete an incident report and inform the healthcare team immediately.
Examples
Example 1: Administering Insulin to a Diabetic Patient
A nurse is tasked with administering subcutaneous insulin to a diabetic patient to control blood glucose levels. The nurse follows the Five Rights of Medication Administration: confirming the right patient using two identifiers, checking the insulin type (e.g., rapid-acting, long-acting) against the prescription, calculating the correct dose, selecting the appropriate route (subcutaneous), and ensuring the insulin is administered at the prescribed time. The nurse also rotates the injection site to prevent lipohypertrophy and educates the patient on proper insulin storage and self-administration.
Example 2: Administering Intravenous (IV) Antibiotics to a Patient with a Bacterial Infection
A patient diagnosed with sepsis requires an IV antibiotic (e.g., vancomycin) to eliminate the bacterial infection. The nurse calculates the correct dose based on the patient’s weight (mg/kg), verifies the infusion rate, and programs the infusion pump accordingly. Before administering the antibiotic, the nurse checks the patient for any known drug allergies and monitors for signs of allergic reactions (e.g., rash, difficulty breathing) during the infusion. The nurse also documents the start time, rate, and any adverse reactions experienced by the patient.
Example 3: Administering Oral Medications to a Pediatric Patient
A nurse is responsible for giving an oral liquid antibiotic (e.g., amoxicillin) to a 5-year-old child. Since pediatric dosing is calculated based on the child’s weight (mg/kg/day), the nurse uses the appropriate pediatric dosage formula to determine the correct dose. The nurse ensures the child is in an upright position to prevent aspiration, measures the liquid using an oral syringe for precision, and provides reassurance to reduce anxiety. After administration, the nurse documents the medication, dose, and time given, as well as any adverse reactions the child may experience.
Example 4: Administering Pain Medication to a Post-Surgical Patient
A post-operative patient is experiencing severe pain and is prescribed an intramuscular (IM) injection of morphine. The nurse follows the Three Checks by verifying the medication name, dose, and expiration date. The nurse prepares the injection using aseptic technique, selects the appropriate muscle site (e.g., deltoid or vastus lateralis), and administers the drug at a 90-degree angle. The nurse observes the patient for potential adverse effects such as respiratory depression, sedation, or hypotension. After administration, the nurse monitors the patient’s pain level and vital signs to ensure the medication is effective and safe.
Example 5: Administering Emergency Epinephrine for Anaphylaxis
A patient develops a severe anaphylactic reaction after exposure to a known allergen (e.g., peanuts or latex). The nurse quickly administers an intramuscular (IM) injection of epinephrine as a life-saving intervention. Adhering to emergency protocols, the nurse ensures that the epinephrine dose (typically 0.3 mg for adults, 0.15 mg for children) is administered into the vastus lateralis muscle. The nurse closely monitors the patient for signs of improvement (e.g., decreased wheezing, improved oxygen saturation) and potential adverse effects such as tachycardia or hypertension. The nurse documents the event, including the time of administration, dose, patient response, and any additional interventions.
Practice Questions
Question 1
A nurse is preparing to administer an oral medication to a patient. Which of the following actions demonstrates adherence to the Five Rights of Medication Administration?
A. The nurse administers the medication to the patient immediately upon entering the room.
B. The nurse confirms the patient’s name and date of birth, checks the medication label three times, and administers the medication via the prescribed route.
C. The nurse checks the medication label once and asks the patient if the medication looks familiar.
D. The nurse asks another nurse to administer the medication on their behalf and assumes the other nurse will follow the correct procedure.
Answer: B
Explanation:
Option B follows the “Five Rights of Medication Administration,” which include:
- Right Patient – The nurse confirms the patient’s identity using two identifiers (name and date of birth).
- Right Drug – The nurse verifies the medication label to ensure it matches the order.
- Right Dose – The nurse ensures the dosage matches the prescription.
- Right Route – The nurse verifies that the drug is administered via the correct route (oral in this case).
- Right Time – The nurse ensures the drug is given at the appropriate time.
The Three Checks (checking the label when removing the drug, before preparing it, and before administration) are also a standard safety protocol. Option A is incorrect because it lacks verification of patient identity or the medication. Option C is incorrect because relying on the patient to identify the medication is unsafe. Option D is incorrect because the nurse remains responsible for any medication administered, even if delegated.
Question 2
A physician orders 500 mg of amoxicillin for a patient. The medication is available in 250 mg tablets. How many tablets should the nurse administer to the patient?
A. 1 tablet
B. 2 tablets
C. 3 tablets
D. 4 tablets
Answer: B
Explanation:
To calculate the number of tablets to administer, the nurse should use the dosage calculation formula:
![]()
Where:
- Desired Dose = 500 mg (the amount prescribed)
- Available Dose = 250 mg (the amount of drug in one tablet)
- Quantity Available = 1 tablet
Dose to Administer=( 500mg/ 250mg ) × 1tablet.
Dose to Administer = 2tablets
Therefore, the nurse should administer 2 tablets to meet the ordered dose of 500 mg.
Option A is incorrect because 1 tablet only provides 250 mg. Option C (3 tablets) would provide 750 mg, which exceeds the prescribed dose. Option D (4 tablets) would provide 1000 mg, which is double the required dose.
Question 3
A patient receiving intravenous (IV) antibiotics begins to experience itching, swelling of the lips, and difficulty breathing. What is the nurse’s priority action?
A. Stop the IV infusion immediately.
B. Administer diphenhydramine (Benadryl) as prescribed.
C. Document the patient’s reaction in the chart.
D. Call the healthcare provider for further instructions.
Answer: A
Explanation: The patient is exhibiting signs of a severe allergic reaction (also known as anaphylaxis), which can be life-threatening. The nurse’s priority action is to stop the IV infusion immediately to prevent more of the allergen from entering the bloodstream. Once the infusion is stopped, the nurse should follow emergency protocols, which often include administering epinephrine and calling for emergency support.
Why the other options are incorrect:
- Option B: Administering diphenhydramine (Benadryl) can help relieve mild allergic reactions like rash or itching but is not a priority in an anaphylactic reaction where airway obstruction is a concern.
- Option C: While documentation is necessary, it is a low-priority action compared to stopping the source of the allergen.
- Option D: Calling the healthcare provider is important, but the nurse should first stop the infusion to prevent further administration of the allergen.