The musculoskeletal system is a vital focus area on the NCLEX-RN®, encompassing disorders affecting bones, muscles, joints, and connective tissues. As a nurse, you must understand common conditions like fractures, arthritis, osteoporosis, and compartment syndrome, along with their management. Key topics include promoting mobility, preventing complications, and patient education on injury prevention and chronic disease management. Questions often assess prioritization, safety interventions, and appropriate nursing care, ensuring you can effectively support patients with musculoskeletal challenges and improve their quality of life.
In studying “Musculoskeletal” for the NCLEX-RN® Exam, you should learn to understand common musculoskeletal disorders, including fractures, osteoporosis, and arthritis, and their associated nursing interventions. Analyze clinical scenarios to recognize complications such as compartment syndrome and fat embolism, and prioritize appropriate nursing actions. Evaluate principles of patient mobility, pain management, and rehabilitation strategies, including physical therapy and assistive device use. Explore pre- and post-operative care for musculoskeletal surgeries like joint replacements. Apply your understanding to interpreting patient care plans, safety measures, and diagnostic findings to address patient needs and improve outcomes in NCLEX practice scenarios.
The musculoskeletal system is integral to understanding patient mobility, stability, and overall health. Questions on the NCLEX-RN® about this system often focus on disease processes, interventions, complications, and patient teaching.
1. Anatomy and Physiology
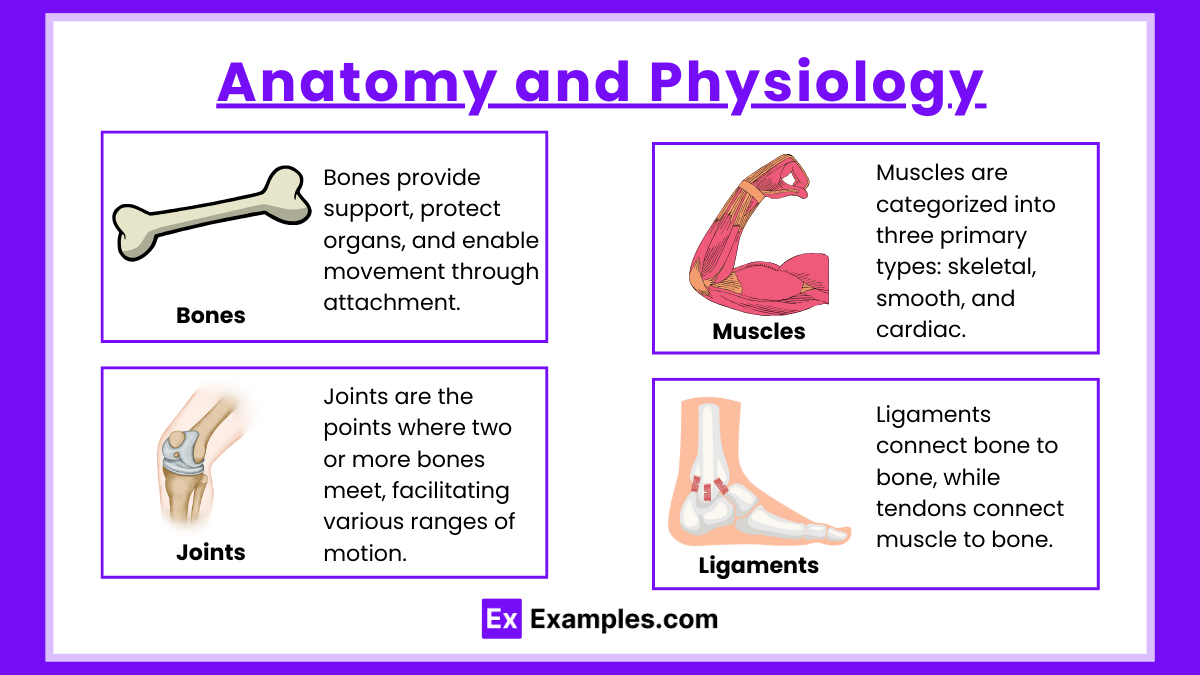
- Bones: Support, protection, mineral storage (calcium and phosphorus), hematopoiesis. Bones play a vital role in the human body by providing structural support, protecting internal organs, and serving as a framework for muscle attachment, enabling movement. They also act as a reservoir for essential minerals such as calcium and phosphorus, which are crucial for metabolic processes and maintaining bone strength. Additionally, bones are involved in hematopoiesis, the production of blood cells, which occurs within the bone marrow.
- Muscles: Types include skeletal (voluntary movement), smooth (involuntary), and cardiac. Muscles are categorized into three primary types: skeletal, smooth, and cardiac. Skeletal muscles are responsible for voluntary movements, such as walking and lifting, and are controlled consciously. They are attached to bones by tendons and work in pairs to produce precise movements.
- Joints: Classified as synovial (freely movable), cartilaginous, or fibrous. Joints are the points where two or more bones meet, facilitating various ranges of motion. They are classified into three main types based on their structure and function. Synovial joints, like the shoulder and knee, are the most mobile and allow movements such as rotation, flexion, and extension.
- Ligaments : Ligaments connect bone to bone, while tendons connect muscle to bone. Ligaments and tendons are connective tissues that play distinct yet complementary roles in maintaining structural integrity and facilitating movement. Ligaments connect bone to bone, stabilizing joints and preventing excessive movement that could lead to injury.
2. Common Disorders of Musculoskeletal
- Fractures: Types include closed/simple, open/compound, comminuted, spiral, and greenstick.
- Signs/Symptoms: Pain, deformity, swelling, decreased function.
- Management: Immobilization, pain management, surgical interventions (ORIF).
- Complications: Fat embolism syndrome (FES), compartment syndrome, infection.
- Osteoarthritis (OA):
- Pathophysiology: Degeneration of articular cartilage.
- Symptoms: Joint pain, stiffness, crepitus.
- Management: NSAIDs, physical therapy, joint replacement.
- Rheumatoid Arthritis (RA):
- Pathophysiology: Autoimmune inflammation of synovium.
- Symptoms: Symmetrical joint swelling, morning stiffness.
- Management: DMARDs (methotrexate), corticosteroids, biologics.
- Osteoporosis:
- Pathophysiology: Decreased bone density.
- Risk Factors: Postmenopause, low calcium/vitamin D, smoking.
- Prevention: Weight-bearing exercises, calcium/vitamin D supplements.
- Treatment: Bisphosphonates, calcitonin.
- Gout:
- Pathophysiology: Uric acid crystal deposition in joints.
- Symptoms: Red, swollen, painful joints (typically the great toe).
- Treatment: NSAIDs, colchicine, allopurinol.
- Amputations:
- Types: Above-knee (AKA), below-knee (BKA).
- Post-op Care: Monitor for infection, phantom limb pain (gabapentin).
- Complications: Contractures, wound care.
3. Diagnostic Tests
- X-rays: Assess bone fractures, deformities.
- MRI: Detect soft tissue injuries, ligament tears.
- DEXA Scan: Measures bone density for osteoporosis.
- Arthroscopy: Direct visualization of joints.
- Bone Biopsy: Diagnose infections or cancers.
Examples
Example 1. Osteoporosis and Fracture Risk
A postmenopausal woman with osteoporosis may present on the NCLEX-RN® as a scenario where the nurse must identify interventions to reduce fracture risk. Questions may ask about promoting weight-bearing exercises, ensuring adequate calcium and vitamin D intake, or recognizing the need for home safety modifications to prevent falls. For example, the nurse might educate the patient to remove rugs, install grab bars, and use proper lighting at home.
Example 2. Compartment Syndrome
An NCLEX question may describe a patient with a recent tibial fracture complaining of severe, unrelenting pain despite medication, accompanied by swelling and numbness. The test might ask for the appropriate nursing action, such as assessing for the “6 Ps” (pain, pallor, pulselessness, paresthesia, paralysis, poikilothermia) and notifying the healthcare provider immediately. This tests the nurse’s ability to recognize an emergent condition requiring fasciotomy to prevent tissue damage.
Example 3. Rheumatoid Arthritis
A patient diagnosed with rheumatoid arthritis (RA) might be presented with symptoms such as joint swelling, pain, and morning stiffness. The NCLEX-RN® could ask about the nurse’s role in managing RA, including teaching the importance of adhering to disease-modifying antirheumatic drugs (DMARDs) like methotrexate, and suggesting low-impact exercises to maintain joint function. Patient education on avoiding triggers and recognizing early signs of flare-ups may also be included.
Example 4. Post-Operative Care for Joint Replacement
The NCLEX-RN® may test the nurse’s knowledge of caring for a patient after total hip or knee replacement surgery. Questions could involve proper positioning to prevent dislocation (e.g., using an abduction pillow after hip replacement), monitoring for signs of infection, and encouraging early ambulation to prevent complications like deep vein thrombosis (DVT). The nurse might also educate the patient on physical therapy and assistive devices for mobility.
Example 5. Gout Management
A patient with gout might appear in a case study format, describing acute joint inflammation, redness, and severe pain in the big toe. NCLEX questions could focus on nursing interventions, such as administering prescribed medications like colchicine or NSAIDs, advising the patient to avoid purine-rich foods (e.g., red meat, shellfish), and encouraging increased hydration to promote uric acid excretion. Education on the importance of compliance with long-term medications like allopurinol to prevent future attacks may also be tested.
Practice Questions
Question 1
A 75-year-old female patient with osteoporosis is admitted to the hospital after falling at home. She reports severe pain in her left hip. X-rays confirm a hip fracture. What is the nurse’s priority intervention?
A. Administer prescribed pain medication.
B. Encourage the patient to ambulate with assistance.
C. Monitor neurovascular status of the affected extremity.
D. Provide the patient with information about fall prevention strategies.
Answer: C. Monitor neurovascular status of the affected extremity.
Explanation: Monitoring neurovascular status (circulation, sensation, and movement) is the priority in this scenario to assess for complications such as impaired blood flow or nerve damage following the fracture. Pain management (Option A) is important but secondary to ensuring there is no compromise in circulation. Encouraging ambulation (Option B) is contraindicated until the fracture is stabilized. Fall prevention strategies (Option D) are a future consideration but not the immediate priority in an acute fracture.
Question 2
A patient with rheumatoid arthritis (RA) is prescribed methotrexate. What statement by the patient indicates the need for further teaching?
A. “I will avoid drinking alcohol while taking this medication.”
B. “I will stop the medication if I feel better to avoid side effects.”
C. “I understand I need regular blood tests to monitor my liver function.”
D. “I will notify my healthcare provider if I have symptoms of infection.”
Answer: B. “I will stop the medication if I feel better to avoid side effects.”
Explanation: Methotrexate is a disease-modifying antirheumatic drug (DMARD) that requires consistent use to manage RA effectively. Stopping the medication without medical advice can lead to a worsening of symptoms and disease progression. Avoiding alcohol (Option A) is correct because methotrexate can cause hepatotoxicity. Regular blood tests (Option C) are necessary for monitoring liver function and bone marrow suppression. Reporting infections (Option D) is vital because methotrexate suppresses the immune system.
Question 3
The nurse is caring for a patient who had a total hip replacement 24 hours ago. Which intervention is most appropriate to prevent complications?
A. Place a pillow under the patient’s knees to elevate the legs.
B. Encourage the patient to perform foot flexion and extension exercises.
C. Assist the patient to sit in a low chair to improve comfort.
D. Allow the patient to cross their legs to prevent stiffness.
Answer: B. Encourage the patient to perform foot flexion and extension exercises.
Explanation: Foot flexion and extension exercises (ankle pumps) are critical to promoting circulation and preventing complications like deep vein thrombosis (DVT) following surgery. Placing a pillow under the knees (Option A) can impair circulation and is contraindicated. Sitting in a low chair (Option C) increases the risk of hip dislocation by exceeding the 90-degree hip flexion limit. Crossing the legs (Option D) is contraindicated as it can also lead to hip dislocation or impaired circulation.