The musculoskeletal system in children is unique due to rapid growth and developmental changes, making it a critical area in pediatric nursing for the NCLEX-RN®. This system includes bones, muscles, and connective tissues, which are susceptible to congenital and acquired disorders. Key conditions like developmental dysplasia of the hip, scoliosis, fractures, and muscular dystrophies require prompt diagnosis and specialized care. Nurses play a vital role in ensuring mobility, managing pain, and educating families. Understanding these disorders enhances patient outcomes and supports success in the exam.
Learning Objectives
In studying "Child Health: Musculoskeletal" for the NCLEX-RN®, you should learn to understand the assessment and management of pediatric musculoskeletal disorders, including developmental dysplasia of the hip (DDH), scoliosis, and fractures. Evaluate the unique characteristics of pediatric bones, growth plates, and their implications for healing and injury. Analyze the principles behind interventions like casting, bracing, and surgical procedures. Explore conditions such as juvenile idiopathic arthritis, muscular dystrophies, and clubfoot, and their impact on mobility and function. Additionally, apply your understanding to prioritize care, recognize complications (e.g., compartment syndrome), and provide patient-centered education for caregivers in clinical practice scenarios.
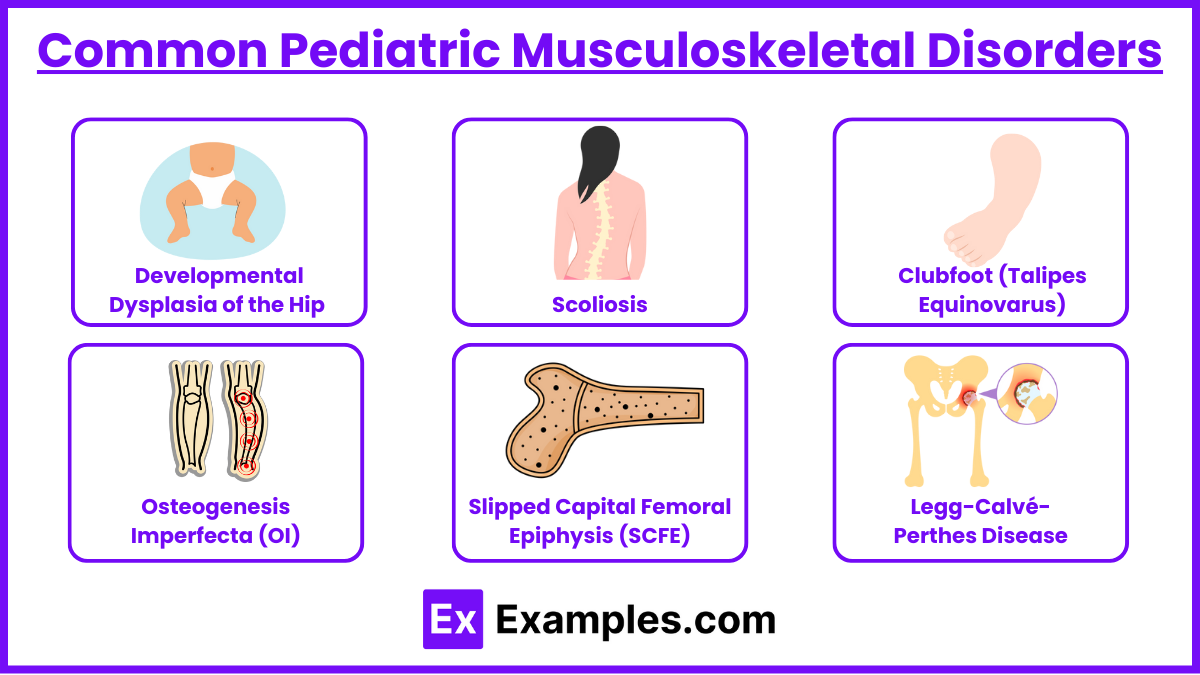
Common Pediatric Musculoskeletal Disorders
The musculoskeletal system in pediatric patients involves bones, muscles, and connective tissues that grow and develop rapidly. Understanding congenital and acquired conditions, as well as treatment plans, is crucial for providing optimal care. This section aligns with NCLEX-RN® test plan categories, especially Management of Care and Physiological Integrity.
Developmental Dysplasia of the Hip (DDH) : A condition where the hip joint does not develop properly, resulting in instability or dislocation of the femoral head from the acetabulum. It may range from a mildly unstable hip to complete dislocation.
Risk Factors: Breech birth, family history, female gender.
Assessment:
Positive Ortolani and Barlow maneuvers.
Asymmetric thigh folds.
Management:
Pavlik harness (<6 months).
Closed reduction and spica casting (>6 months).
Scoliosis : A lateral curvature of the spine greater than 10 degrees, often accompanied by vertebral rotation. It can be idiopathic, congenital, or neuromuscular in origin.
Assessment:
Adam’s forward bend test.
Uneven shoulders/hips.
Management:
Bracing (mild curvature).
Surgical intervention (severe cases >40 degrees).
Clubfoot (Talipes Equinovarus) : A congenital deformity characterized by inward turning of the foot and ankle, often involving plantar flexion, inversion, and adduction of the forefoot.
Assessment:
Inward turning of the foot.
Management:
Serial casting (Ponseti method).
Surgery if unresponsive to casting.
Osteogenesis Imperfecta (OI) : A genetic disorder resulting in brittle bones due to defective collagen production, making individuals prone to fractures. It is also known as "brittle bone disease."
Assessment:
Frequent fractures.
Blue sclera, hearing loss.
Management:
Bisphosphonate therapy.
Gentle handling and physical therapy.
Slipped Capital Femoral Epiphysis (SCFE) : A condition in which the femoral head slips posteriorly and inferiorly at the growth plate, leading to hip pain and gait abnormalities, most commonly in adolescents.
Risk Factors: Obesity, adolescence.
Assessment:
Limping, hip/groin/knee pain.
Management:
Surgical fixation (pinning).
Legg-Calvé-Perthes Disease: A childhood condition characterized by avascular necrosis of the femoral head due to temporary disruption of blood supply. This leads to bone death and subsequent regeneration, often causing hip pain and gait abnormalities.
Assessment:
Limping (painless or painful).
Limited range of motion in the hip.
Hip, thigh, or knee pain.
Management:
Rest and activity modification.
Physical therapy to maintain hip mobility.
Orthopedic interventions (e.g., bracing or surgery) in severe cases.
Fractures in Children
Fractures in children are unique because of their growing bones, which have different mechanical properties and repair processes compared to adult bones. The presence of growth plates (physes) and the ability to remodel give pediatric fractures distinct patterns and considerations in treatment.
Unique Features:
Growth plate involvement (physeal fractures).Fractures involving the growth plate can affect bone growth and result in deformities if not treated properly.
Bone remodeling potential. Children's bones can remodel with time, allowing for better correction of angular deformities.
Common Types:
Greenstick fracture : An incomplete fracture where the bone bends on one side and cracks on the other.
Spiral fracture (possible child abuse) : May indicate possible child abuse, especially in non-ambulatory children.
Management:
Immobilize the injured limb using splints or temporary casts to prevent further injury. Apply ice packs and elevate the limb to reduce swelling.
Monitor for complications (compartment syndrome).
Juvenile Idiopathic Arthritis (JIA)
Juvenile Idiopathic Arthritis (JIA) is the most common chronic rheumatologic condition in children, characterized by persistent joint inflammation. It affects children under the age of 16 and is classified into subtypes based on the number of joints involved and associated symptoms.
Types:
Oligoarticular (1-4 joints).
Polyarticular (>5 joints).
Assessment:
Joint swelling, pain, and stiffness.
Morning stiffness.
Management:
NSAIDs, DMARDs (e.g., methotrexate).
Physical therapy, regular exercise.
Muscular Dystrophies

Muscular dystrophies (MD) are a group of genetic disorders characterized by progressive muscle weakness and degeneration due to defects in muscle protein production. Among the various types, Duchenne Muscular Dystrophy (DMD) and Becker Muscular Dystrophy (BMD) are the most common in pediatric populations. These conditions are critical for the NCLEX-RN® as they often involve comprehensive care planning.
Duchenne Muscular Dystrophy (DMD) : DMD is an X-linked recessive disorder caused by mutations in the dystrophin gene, which leads to an absence of dystrophin, a protein critical for muscle strength and function. It primarily affects boys, with symptoms appearing around ages 2–5 years.
X-linked recessive disorder.
Progressive muscle weakness.
Positive Gower’s sign.
Management:
The management of Duchenne Muscular Dystrophy is multifaceted, focusing on slowing disease progression, maximizing functional abilities, and providing supportive care to improve quality of life. Corticosteroids to slow progression.
Supportive care (mobility aids, respiratory support).
Examples
Example 1: Developmental Dysplasia of the Hip (DDH)
This congenital condition involves abnormal development or dislocation of the hip joint. It is often detected in infancy through asymmetrical gluteal folds, limited hip abduction, or positive Ortolani and Barlow tests. Early treatment, such as using a Pavlik harness, is crucial to ensure proper joint alignment and avoid long-term complications like gait abnormalities. For older children, surgical intervention and spica casting may be required.
Example 2: Scoliosis
A lateral curvature of the spine, scoliosis is often identified during school-age growth spurts. Mild cases are managed with observation, while moderate curvatures may require bracing to prevent progression. Severe cases (curvatures >40 degrees) often necessitate surgical intervention, such as spinal fusion. Nurses play a vital role in patient education, ensuring compliance with bracing, and monitoring for complications post-surgery.
Example 3: Clubfoot (Talipes Equinovarus)
Clubfoot is a congenital deformity where the foot turns inward and downward. Early intervention, typically through serial casting using the Ponseti method, is critical to correcting the deformity. In cases where casting fails, surgical correction may be necessary. Nurses educate parents on cast care, signs of neurovascular compromise, and the importance of follow-up appointments.
Example 4: Juvenile Idiopathic Arthritis (JIA)
This autoimmune disorder causes chronic joint inflammation, leading to pain, swelling, and stiffness, particularly in the morning. Management includes NSAIDs, DMARDs like methotrexate, and physical therapy to maintain joint mobility. Nurses support patients and families by teaching medication administration, promoting exercise, and emphasizing the importance of regular ophthalmologic exams due to the risk of uveitis.
Example 5: Duchenne Muscular Dystrophy (DMD)
An X-linked genetic disorder, DMD is characterized by progressive muscle weakness due to the absence of dystrophin protein. Symptoms often appear in early childhood, with difficulty climbing stairs, frequent falls, and a positive Gower’s sign. There is no cure, but corticosteroids may slow progression, and physical therapy can improve quality of life. Nurses focus on preventing complications, such as contractures and respiratory decline, while providing emotional support to families coping with the progressive nature of the disease.
Practice Questions
Question 1
A 6-month-old infant is diagnosed with Developmental Dysplasia of the Hip (DDH). The nurse should anticipate which intervention?
A. Administer calcium supplements.
B. Apply a Pavlik harness.
C. Prepare the child for surgical intervention.
D. Teach the parents about spica cast care.
Answer: B. Apply a Pavlik harness.
Explanation:
Developmental Dysplasia of the Hip (DDH) involves improper alignment of the femoral head with the acetabulum, leading to hip instability.
Infants under 6 months old are typically treated with a Pavlik harness, which keeps the hips flexed and abducted, promoting proper joint development.
Why not A? Calcium supplements are not relevant for treating DDH.
Why not C? Surgical intervention is reserved for older children or if conservative measures fail.
Why not D? Spica casts are used after surgical correction in children older than 6 months.
Question 2
A school nurse is assessing a 12-year-old girl who reports back pain and uneven shoulders. On examination, the nurse observes a rib hump when the child bends forward. What is the most likely condition?
A. Scoliosis
B. Kyphosis
C. Lordosis
D. Spina bifida
Answer: A. Scoliosis
Explanation:
Scoliosis is a lateral curvature of the spine often detected in adolescence during growth spurts.
A hallmark sign is the rib hump or asymmetry in the shoulders and hips, particularly visible when the child performs a forward bend test (Adam’s test).
Why not B? Kyphosis is characterized by excessive forward curvature of the thoracic spine (hunchback).
Why not C? Lordosis involves excessive inward curvature of the lumbar spine.
Why not D? Spina bifida is a neural tube defect present at birth and not associated with rib humps or postural changes in adolescence.
Question 3
A 7-year-old boy with osteogenesis imperfecta (OI) is hospitalized after a minor fall resulting in a fractured arm. Which nursing intervention is most appropriate?
A. Perform passive range-of-motion exercises on the affected arm.
B. Handle the child carefully to minimize additional fractures.
C. Encourage participation in high-impact sports for bone strengthening.
D. Withhold all pain medications to prevent masking symptoms.
Answer: B. Handle the child carefully to minimize additional fractures.
Explanation:
Osteogenesis imperfecta (OI) is a genetic condition causing brittle bones that fracture easily, even with minimal trauma.
Gentle handling is essential to prevent additional fractures.
Why not A? Passive range-of-motion exercises are contraindicated on a fractured limb as they can worsen the injury.
Why not C? High-impact activities increase the risk of fractures in children with OI. Low-impact activities like swimming are recommended.
Why not D? Pain management is critical in children with fractures and should not be withheld.