The neurologic system is a critical area in the NCLEX-RN® exam, assessing your ability to manage disorders affecting the brain, spinal cord, and nerves. Key topics include stroke, increased intracranial pressure, seizures, meningitis, and degenerative conditions like Parkinson’s disease. Success on the exam requires proficiency in neurologic assessment, recognizing early warning signs, and prioritizing interventions. Focus on safety precautions, effective communication, and patient education. Understanding these concepts ensures you can deliver high-quality, patient-centered care and excel in your NCLEX preparation.
Learning Objectives
In studying “Neurologic” for the NCLEX-RN®, you should learn to understand the assessment and management of neurologic conditions, including stroke, seizures, and increased intracranial pressure. Analyze key neurologic assessment techniques, such as the Glasgow Coma Scale, cranial nerve testing, and monitoring for Cushing’s Triad. Evaluate interventions for conditions like meningitis, Parkinson’s disease, and traumatic brain injuries, emphasizing airway management, safety precautions, and medication administration. Additionally, explore how neurologic disorders impact overall patient care, focusing on prioritizing interventions, patient education, and interpreting clinical symptoms to ensure effective, evidence-based care in diverse healthcare scenarios.
Neurologic System
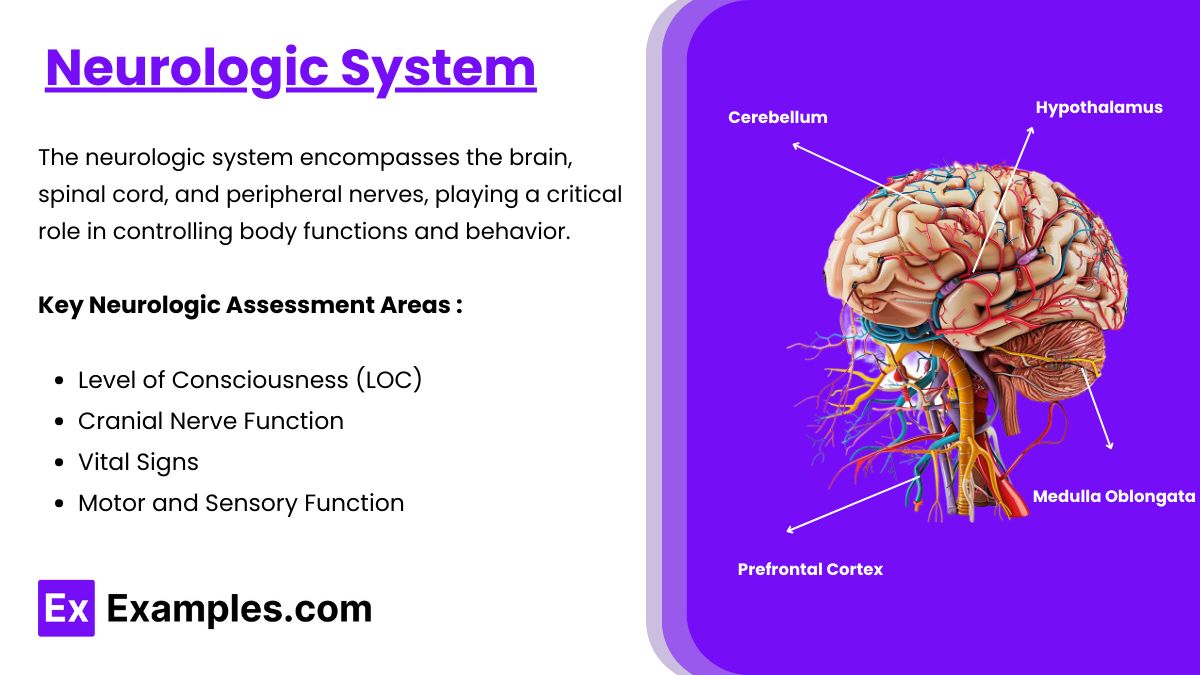
The neurologic system encompasses the brain, spinal cord, and peripheral nerves, playing a critical role in controlling body functions and behavior. Key focus areas include neurologic assessments like the Glasgow Coma Scale (GCS) to evaluate consciousness, and cranial nerve testing. Common neurologic conditions include stroke, increased intracranial pressure (ICP), seizures, meningitis, and Parkinson’s disease. Nurses must identify life-threatening signs such as altered LOC, Cushing’s Triad, or seizure activity. Management involves interventions like head elevation for ICP, thrombolytics for ischemic strokes, and antiepileptic drugs for seizures. Emphasizing safety measures, such as seizure precautions and aspiration prevention, alongside patient education, ensures comprehensive care.
Key Neurologic Assessment Areas
- Level of Consciousness (LOC): Assess using the Glasgow Coma Scale (GCS) – Score ranges from 3 (deep coma) to 15 (normal).
- Eye Opening: Spontaneous, to speech, to pain, or none.
- Verbal Response: Oriented, confused, inappropriate words, incomprehensible sounds, or none.
- Motor Response: Follows commands, localizes pain, withdraws, abnormal flexion (decorticate), abnormal extension (decerebrate), or none.
- Cranial Nerve Function: Test all 12 cranial nerves, focusing on:
- Pupillary response (CN II, III) – PERRLA (Pupils Equal, Round, Reactive to Light and Accommodation).
- Swallowing and gag reflex (CN IX, X).
- Vital Signs: Watch for Cushing’s Triad (increased BP, bradycardia, irregular respirations) – a sign of increased intracranial pressure (ICP).
- Motor and Sensory Function:
- Strength grading (0-5 scale).
- Assess for symmetry and coordination.
- Check reflexes (e.g., deep tendon reflexes) and sensation to touch and pain.
Neurologic Disorders
- Brain Stroke (Cerebrovascular Accident – CVA):
- Types: Ischemic (thrombotic, embolic) vs. Hemorrhagic.
- Signs and Symptoms: FAST (Face drooping, Arm weakness, Speech difficulty, Time to call 911).
- Management:
- Ischemic: Thrombolytics (tPA) within 3-4.5 hours if eligible.
- Hemorrhagic: Monitor ICP, avoid anticoagulants, prepare for surgery if needed.
- Nursing Priorities: Elevate head of bed 30 degrees, maintain airway, prevent aspiration.
- Increased Intracranial Pressure (ICP):
- Causes: Trauma, hemorrhage, tumors, infections.
- Symptoms: Headache, vomiting, decreased LOC, pupil changes.
- Interventions:
- Maintain head elevation at 30 degrees.
- Avoid hip flexion or anything that increases ICP.
- Administer osmotic diuretics (e.g., Mannitol).
- Seizures and Epilepsy:
- Types: Generalized (tonic-clonic, absence) vs. Focal.
- Nursing Care During Seizure:
- Protect the airway, position side-lying, ensure safety.
- Document onset, duration, and activity.
- Postictal Care: Reassess LOC, check for injuries.
- Medications: Phenytoin, levetiracetam.
- Meningitis:
- Signs and Symptoms: Fever, nuchal rigidity, photophobia, positive Kernig’s and Brudzinski’s signs.
- Management:
- Administer antibiotics promptly (bacterial).
- Isolation precautions if required.
- Monitor for signs of septicemia.
- Parkinson’s Disease:
- Symptoms: Tremors, rigidity, bradykinesia, postural instability.
- Interventions:
- Promote physical activity and mobility.
- Administer medications like levodopa/carbidopa.
Key Neurologic Nursing Interventions
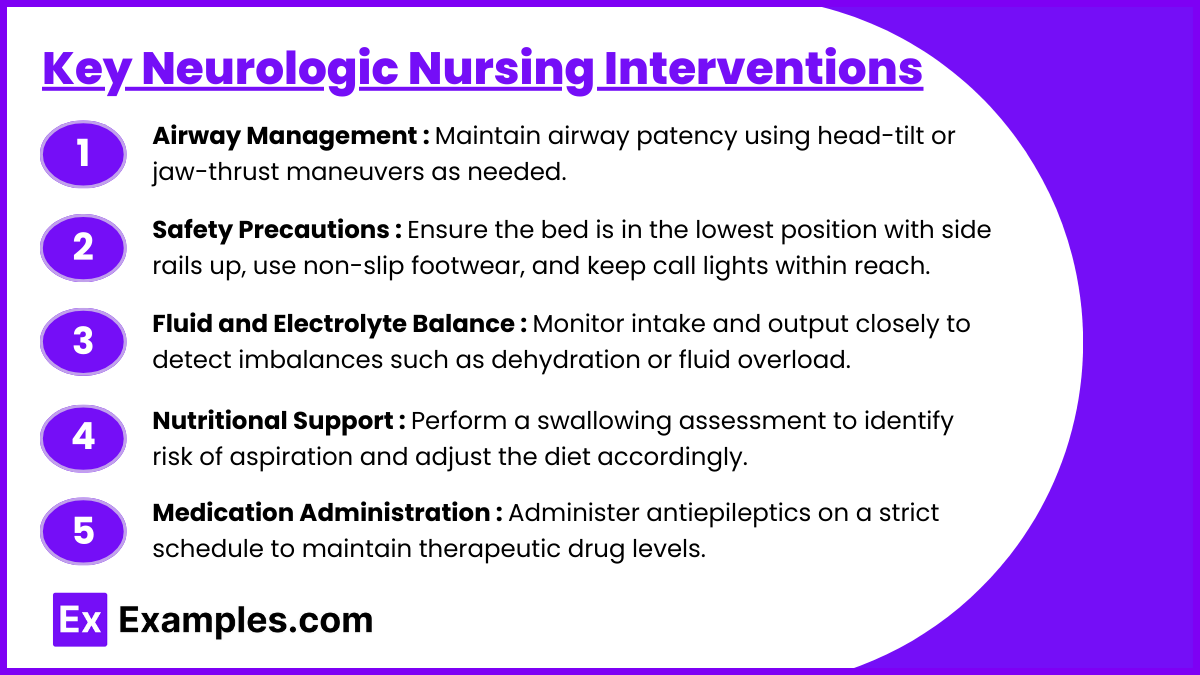
- Airway Management:
- Maintain airway patency using head-tilt or jaw-thrust maneuvers as needed.
- Regularly assess for obstructions like secretions or edema, and suction as necessary to clear the airway.
- Monitor oxygenation with pulse oximetry, ensuring SpO₂ remains above 94%.
- Administer supplemental oxygen or use advanced airway techniques like endotracheal intubation for compromised patients.
- Implement chest physiotherapy if indicated to improve airway clearance.
- Safety Precautions:
- Fall Prevention: Ensure the bed is in the lowest position with side rails up, use non-slip footwear, and keep call lights within reach.
- Seizure Precautions: Place padding around bed rails, ensure oxygen and suction are available, and educate family or caregivers about what to do during a seizure.
- Assess the environment for tripping hazards, such as loose rugs or wires, and remove them.
- Educate patients and families about recognizing triggers for seizures or falls.
- Fluid and Electrolyte Balance:
- Monitor intake and output closely to detect imbalances such as dehydration or fluid overload.
- Regularly check electrolyte levels, particularly sodium, potassium, and calcium, as imbalances can affect neurologic function.
- Administer IV fluids based on the patient’s condition (e.g., isotonic fluids for dehydration, hypertonic saline for hyponatremia).
- Watch for signs of complications like edema, crackles in the lungs, or changes in urine output.
- Educate patients on adequate hydration and dietary sources of essential electrolytes.
- Nutritional Support:
- Perform a swallowing assessment to identify risk of aspiration and adjust the diet accordingly.
- Provide thickened liquids and soft, easy-to-swallow foods for patients with dysphagia.
- Collaborate with a dietitian to ensure nutritional needs are met while adhering to restrictions, such as low sodium or high-protein diets.
- Implement feeding tube care for patients unable to eat orally, ensuring the tube placement is correct and the site is clean.
- Encourage small, frequent meals for patients with fatigue or reduced appetite.
- Medication Administration:
- Administer antiepileptics (e.g., phenytoin, levetiracetam) on a strict schedule to maintain therapeutic drug levels.
- Use thrombolytics like alteplase (tPA) for ischemic stroke within the time window while closely monitoring for bleeding risks.
- Prescribe diuretics (e.g., mannitol) for patients with increased ICP, observing for electrolyte imbalances or dehydration.
- Administer muscle relaxants for spasticity in conditions like multiple sclerosis or spinal cord injuries.
- Monitor patients for medication side effects, such as drowsiness with antiepileptics or hypotension with diuretics, and educate them about adherence and signs of adverse effects.
Examples
Example 1: Stroke (Cerebrovascular Accident – CVA) Management
A patient arrives in the emergency department with symptoms of facial drooping, arm weakness, and slurred speech. The nurse prioritizes assessing the time of symptom onset to determine eligibility for thrombolytic therapy (tPA) in ischemic stroke. The intervention plan includes elevating the head of the bed, administering prescribed antihypertensives, and monitoring for signs of increased intracranial pressure.
Example 2: Seizure Precautions and Care
A patient with a history of epilepsy experiences a generalized tonic-clonic seizure during their hospital stay. The nurse protects the patient by ensuring a side-lying position, providing a padded bed environment, and noting the seizure duration and activity. Postictal care focuses on reorienting the patient, checking for injuries, and administering antiepileptic medications as prescribed.
Example 3: Increased Intracranial Pressure (ICP) Management
A patient with a traumatic brain injury exhibits symptoms of severe headache, vomiting, and decreased level of consciousness. The nurse implements interventions to reduce ICP, such as elevating the head of the bed to 30 degrees, maintaining a quiet environment, and administering osmotic diuretics like Mannitol. Continuous monitoring for Cushing’s Triad (hypertension, bradycardia, irregular respirations) is performed.
Example 4: Parkinson’s Disease Nursing Care
A patient diagnosed with Parkinson’s disease presents with tremors, bradykinesia, and postural instability. The nurse collaborates with the physical therapy team to promote safe mobility, educates the patient on medication timing for levodopa/carbidopa to maximize symptom control, and monitors for complications such as aspiration or fall risk due to impaired balance.
Example 5: Meningitis Precautions and Treatment
A patient with fever, nuchal rigidity, and photophobia is suspected of having bacterial meningitis. The nurse initiates droplet isolation precautions, collects cerebrospinal fluid (CSF) samples via lumbar puncture, and administers prescribed antibiotics promptly. Frequent monitoring for neurologic status changes and septicemia is performed to prevent complications.
Practice Questions
Question 1
A patient presents to the emergency department with slurred speech, facial drooping, and weakness in the right arm that began 1.5 hours ago. What is the nurse’s priority action?
A. Obtain a complete medical history.
B. Perform a complete neurologic assessment.
C. Administer prescribed thrombolytic therapy (tPA).
D. Ensure a computed tomography (CT) scan is performed.
Answer: D. Ensure a computed tomography (CT) scan is performed.
Explanation: For suspected stroke patients, determining whether the stroke is ischemic or hemorrhagic is critical before initiating any treatment like thrombolytic therapy (tPA). A CT scan helps identify the type of stroke. Administering tPA without confirming the absence of hemorrhage could worsen the condition. Neurologic assessment and obtaining medical history are important but secondary to imaging. Thrombolytic therapy is time-sensitive and only applicable in ischemic strokes within a 3-4.5 hour window.
Question 2
During a patient’s generalized tonic-clonic seizure, which nursing intervention is most appropriate?
A. Place a tongue blade in the patient’s mouth to prevent injury.
B. Restrain the patient to prevent movement and injury.
C. Protect the patient’s head and remove surrounding objects.
D. Administer intravenous antiepileptic medication immediately.
Answer: C. Protect the patient’s head and remove surrounding objects.
Explanation: Safety is the primary focus during a seizure. Protecting the patient’s head and clearing the area to prevent injury are essential. Inserting objects into the mouth or restraining the patient is contraindicated, as these actions can cause further harm. Administering medication is usually done post-seizure unless there are prolonged or repeated seizures (status epilepticus), requiring immediate medical intervention.
Question 3
A patient with a traumatic brain injury has a Glasgow Coma Scale (GCS) score of 8, systolic blood pressure of 180 mmHg, bradycardia, and irregular respirations. What is the priority nursing action?
A. Elevate the head of the bed to 90 degrees.
B. Notify the healthcare provider immediately.
C. Administer prescribed antihypertensive medication.
D. Perform a complete neurologic assessment.
Answer: B. Notify the healthcare provider immediately.
Explanation: The patient is showing signs of Cushing’s Triad (hypertension, bradycardia, and irregular respirations), which indicates increased intracranial pressure and impending brain herniation. This is a medical emergency that requires immediate intervention, such as placement of an intracranial pressure monitoring device or surgical decompression. Elevating the head of the bed to 90 degrees could worsen perfusion, and administering antihypertensives without addressing the ICP could be harmful. A neurologic assessment is ongoing but not the priority in this critical situation.