Newborn care is a critical aspect of maternal and newborn health, focusing on the initial hours to weeks after birth. This period is crucial for the newborn’s adaptation to extrauterine life, involving significant physiological changes such as respiratory and cardiovascular adjustments, thermoregulation, and nutrition. Comprehensive nursing care includes accurate assessments, addressing common complications like hypoglycemia and jaundice, and ensuring parental education on newborn safety and care. Mastery of these concepts is essential for the NCLEX-RN® to deliver effective, evidence-based neonatal care.
Learning Objectives
In studying "Maternal & Newborn Health: Newborn" for the NCLEX-RN® exam, you should learn to understand the physiological adaptations of the newborn to extrauterine life, including respiratory, cardiovascular, and thermoregulatory changes. Analyze the importance of initial newborn assessments such as the Apgar score and physical examination. Evaluate common complications like hypoglycemia, hyperbilirubinemia, and respiratory distress syndrome, along with their nursing management. Explore preventive care, including vitamin K administration, immunizations, and cord care. Additionally, focus on safe sleep practices, parental education, and newborn feeding techniques, and apply this understanding to prioritizing care and interpreting scenarios in NCLEX-RN® practice questions.
1. Physiological Adaptations to Extrauterine Life
The newborn phase is critical for ensuring the transition from intrauterine to extrauterine life is smooth and complication-free. Below is an expanded guide with detailed content to help you thoroughly prepare for the NCLEX-RN® Exam.
Respiratory Adaptations
The first breath clears fluid from the lungs and establishes functional residual capacity.
Surfactant reduces surface tension in alveoli, preventing collapse and promoting oxygen exchange.
Abnormal findings: grunting, nasal flaring, and intercostal retractions indicate respiratory distress.
Cardiovascular Adaptations
Closure of fetal shunts occurs:
Foramen ovale: Closes due to increased left atrial pressure.
Ductus arteriosus: Closes with increased oxygenation.
Ductus venosus: Closes as the umbilical cord is clamped.
Thermoregulation Challenges
Mechanisms of Heat Loss:
Conduction: Direct contact with cold surfaces.
Convection: Heat loss to surrounding cool air.
Evaporation: Loss when liquid evaporates from the skin.
Radiation: Heat loss to nearby cool surfaces without direct contact.
Nursing Interventions:
Dry the baby immediately after birth.
Place under a radiant warmer or initiate skin-to-skin contact.
2. Initial Newborn Assessment and Care
Apgar Scoring
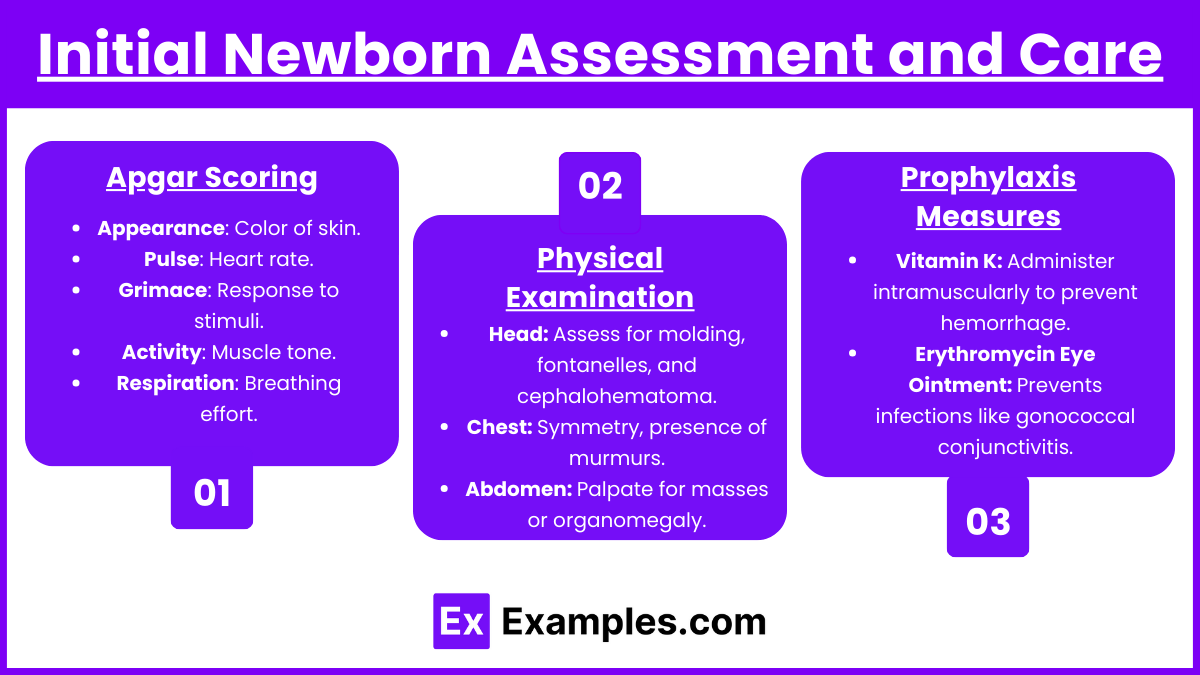
Performed at 1 and 5 minutes post-birth.
Score Breakdown:
Appearance: Color of skin.
Pulse: Heart rate.
Grimace: Response to stimuli.
Activity: Muscle tone.
Respiration: Breathing effort.
Physical Examination
Head: Assess for molding, fontanelles, and cephalohematoma.
Chest: Symmetry, presence of murmurs.
Abdomen: Palpate for masses or organomegaly.
Extremities: Symmetry and range of motion.
Prophylaxis Measures
Vitamin K: Administer intramuscularly to prevent hemorrhage.
Erythromycin Eye Ointment: Prevents infections like gonococcal conjunctivitis.
Hepatitis B Vaccine: Initiate immunization schedule.
3. Common Complications and Nursing Interventions
Hypoglycemia
Common in infants of diabetic mothers or preterm newborns.
Symptoms: Jitteriness, weak cry, poor feeding, and lethargy.
Interventions: Early feeding, IV glucose if severe.
Hyperbilirubinemia (Jaundice)
Physiological Jaundice: Peaks at 3-5 days and resolves without treatment.
Pathological Jaundice: Appears within the first 24 hours; requires intervention.
Treatment: Phototherapy (use eye protection), hydration, monitor bilirubin levels.
Respiratory Distress Syndrome (RDS)
Occurs in preterm infants due to surfactant deficiency.
Symptoms: Cyanosis, grunting, nasal flaring, and retractions.
Management: Administer exogenous surfactant, oxygen therapy, and CPAP.
Infections
Early-onset sepsis often caused by Group B Streptococcus (GBS).
Symptoms: Lethargy, temperature instability, poor feeding.
Interventions: Blood cultures, IV antibiotics.
Examples
Example 1: Apgar Scoring and Immediate Newborn Care
A newborn is delivered at term with a cry immediately after birth. The nurse observes pink skin, a heart rate of 140 bpm, active movement, and a vigorous cry. Apgar scores are calculated at 1 and 5 minutes, scoring 9 each time. The nurse ensures thermoregulation by drying the baby, placing the baby skin-to-skin with the mother, and covering them with a warm blanket. Erythromycin ointment and vitamin K are administered per protocol.
Example 2: Hypoglycemia in a Large for Gestational Age (LGA) Newborn
A 9 lb 5 oz (4.2 kg) newborn is born to a mother with gestational diabetes. Within the first hour, the newborn shows jitteriness, a weak cry, and lethargy. Blood glucose is measured at 35 mg/dL. The nurse initiates early breastfeeding to stabilize glucose levels and closely monitors for further symptoms. If hypoglycemia persists, glucose gel or IV dextrose is administered according to the facility protocol.
Example 3: Hyperbilirubinemia Management in a 3-Day-Old Newborn
A full-term newborn is brought in for evaluation due to yellowing of the skin and sclera noted on day 3. Bilirubin levels are measured at 18 mg/dL. The nurse educates the parents on phototherapy and initiates treatment by placing the baby under phototherapy lights, ensuring the baby’s eyes are protected. Hydration is encouraged through breastfeeding every 2–3 hours, and bilirubin levels are monitored daily.
Example 4: Respiratory Distress Syndrome (RDS) in a Preterm Infant
A 32-week preterm newborn exhibits signs of respiratory distress, including nasal flaring, grunting, and intercostal retractions. The nurse places the newborn in a radiant warmer, provides oxygen therapy via CPAP, and monitors oxygen saturation levels. Surfactant replacement therapy is administered as prescribed. The nurse educates the family about the condition and expected outcomes.
Example 5: Parent Education on Safe Sleep Practices
A nurse is educating first-time parents about reducing the risk of Sudden Infant Death Syndrome (SIDS). The newborn is placed on their back to sleep in a bassinet without blankets, pillows, or toys. The nurse emphasizes using a firm mattress and ensuring the baby sleeps in the same room as the parents, but not in the same bed. The parents are instructed on recognizing signs of illness and the importance of regular pediatric check-ups.
Practice Questions
Question 1
A nurse is assessing a newborn at 5 minutes after birth. The baby is pink with a heart rate of 120 bpm, has active movement, a strong cry, and grimaces in response to a nasal suction. What is the Apgar score for this newborn?
A. 7
B. 8
C. 9
D. 10
Answer: C. 9
Explanation:
The Apgar score evaluates the newborn’s adaptation to extrauterine life at 1 and 5 minutes after birth. Each category scores 0–2 points:
Appearance (Color): Pink (2 points).
Pulse (Heart Rate): 120 bpm (>100 bpm = 2 points).
Grimace (Reflex Irritability): Grimaces (1 point).
Activity (Muscle Tone): Active movement (2 points).
Respiration: Strong cry (2 points).
Total: 2 + 2 + 1 + 2 + 2 = 9.
The score indicates the newborn is transitioning well with no significant distress.
Question 2
A full-term newborn has a bilirubin level of 14 mg/dL on the second day of life. Which of the following actions should the nurse take first?
A. Initiate phototherapy.
B. Feed the newborn formula every 3 hours.
C. Encourage breastfeeding every 2–3 hours.
D. Perform a serum bilirubin test in 4 hours.
Answer: C. Encourage breastfeeding every 2–3 hours.
Explanation:
Physiological Jaundice is common in newborns and peaks at 3–5 days. Adequate feeding promotes excretion of bilirubin via stools and urine.
Breastfeeding every 2–3 hours enhances hydration and stool output, reducing bilirubin levels.
Phototherapy (A) may be indicated for levels >15 mg/dL in term newborns, but feeding is prioritized at 14 mg/dL.
Formula feeding (B) can supplement hydration if breastfeeding is insufficient, but breastfeeding should remain encouraged.
Delaying intervention (D) risks bilirubin rising further.
Question 3
A nurse observes a newborn with grunting, nasal flaring, and intercostal retractions. What is the priority nursing intervention?
A. Administer oxygen via nasal cannula.
B. Perform chest physiotherapy.
C. Place the newborn in skin-to-skin contact with the mother.
D. Assess blood glucose levels.
Answer: A. Administer oxygen via nasal cannula.
Explanation:
Grunting, nasal flaring, and retractions indicate respiratory distress syndrome (RDS), often seen in preterm infants due to surfactant deficiency. Oxygen therapy stabilizes oxygen saturation and prevents hypoxia.
Chest physiotherapy (B) is not appropriate for respiratory distress in neonates.
Skin-to-skin contact (C) supports thermoregulation but is not a priority in respiratory distress.
Blood glucose (D) assessment may be necessary, but respiratory stabilization takes precedence.