The postpartum period, or puerperium, begins immediately after childbirth and lasts about six weeks, marking the transition from pregnancy to recovery. During this time, the mother undergoes significant physiological and psychological changes, including uterine involution, hormonal adjustments, and emotional adaptation. Postpartum care focuses on monitoring the mother’s health, promoting infant bonding, and preventing complications like hemorrhage or infection. Nurses play a vital role in assessing maternal well-being, providing education on self-care, and offering emotional support to ensure a smooth recovery for both mother and baby.
Learning Objectives
In studying “Maternal & Newborn Health: Postpartum” for the NCLEX-RN® Exam, you should learn to understand the physiological and psychological adaptations that occur in the postpartum period, including uterine involution, lochia progression, and emotional changes. Evaluate the principles behind assessments such as the BUBBLE-HE framework and recognize warning signs of complications like postpartum hemorrhage, infection, or depression. Analyze nursing interventions to promote recovery, bonding, and breastfeeding. Explore the role of patient education in ensuring safety and addressing common postpartum challenges. Apply this knowledge to interpret patient scenarios and prioritize care in NCLEX-RN® practice questions.
1. Postprtum Physiological Adaptations
The postpartum period, also known as the puerperium, begins immediately after childbirth and lasts about 6 weeks. It involves physiological and psychological adaptations as the mother transitions from pregnancy to recovery. Below are detailed notes on postpartum care to help you excel in the NCLEX-RN® Exam.
Uterus (Involution)
- Involution Process:
- Uterus returns to pre-pregnancy size through contractions and autolysis.
- Fundus descends 1 cm per day and is no longer palpable after 10–14 days.
- Assessment of Fundus:
- Ensure firmness; a boggy uterus indicates uterine atony and risk for hemorrhage.
- Position: Midline (displacement may suggest a full bladder).
Lochia
- Types and Duration:
- Lochia Rubra: Bright red, lasts 1–3 days.
- Lochia Serosa: Pinkish-brown, lasts 4–10 days.
- Lochia Alba: Whitish-yellow, lasts up to 6 weeks.
- Abnormal Findings:
- Foul odor, heavy bleeding, or large clots may indicate infection or retained placental fragments.
Breasts and Lactation
- Engorgement:
- Occurs around 3–5 days postpartum as milk production begins.
- Nursing mothers: Encourage frequent breastfeeding.
- Non-nursing mothers: Use cold packs and a supportive bra.
- Nipple Care:
- Assess for cracks, redness, or pain; improper latch may cause damage.
Cardiovascular Changes
- Blood volume normalizes through diuresis and diaphoresis.
- Monitor for postpartum hemorrhage (PPH), defined as blood loss >500 mL (vaginal) or >1,000 mL (C-section).
Other Adaptations
- Gastrointestinal: Appetite returns quickly; constipation is common due to decreased motility.
- Urinary: Risk of urinary retention and infection due to trauma or overdistention during labor.
- Musculoskeletal: Gradual return of abdominal muscle tone; diastasis recti may persist.
2. Psychological and Emotional Adaptations
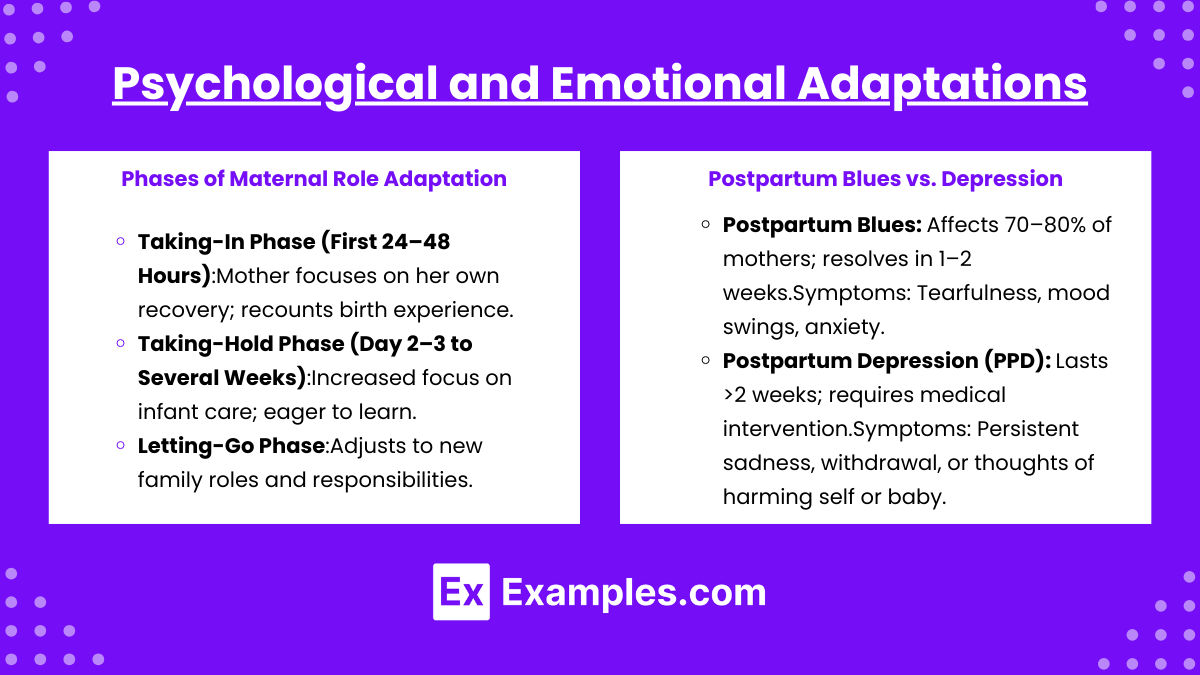
Phases of Maternal Role Adaptation
- Taking-In Phase (First 24–48 Hours):
- Mother focuses on her own recovery; recounts birth experience.
- Taking-Hold Phase (Day 2–3 to Several Weeks):
- Increased focus on infant care; eager to learn.
- Letting-Go Phase:
- Adjusts to new family roles and responsibilities.
Postpartum Blues vs. Depression
- Postpartum Blues: Affects 70–80% of mothers; resolves in 1–2 weeks.
- Symptoms: Tearfulness, mood swings, anxiety.
- Postpartum Depression (PPD): Lasts >2 weeks; requires medical intervention.
- Symptoms: Persistent sadness, withdrawal, or thoughts of harming self or baby.
3. Nursing Assessment and Interventions
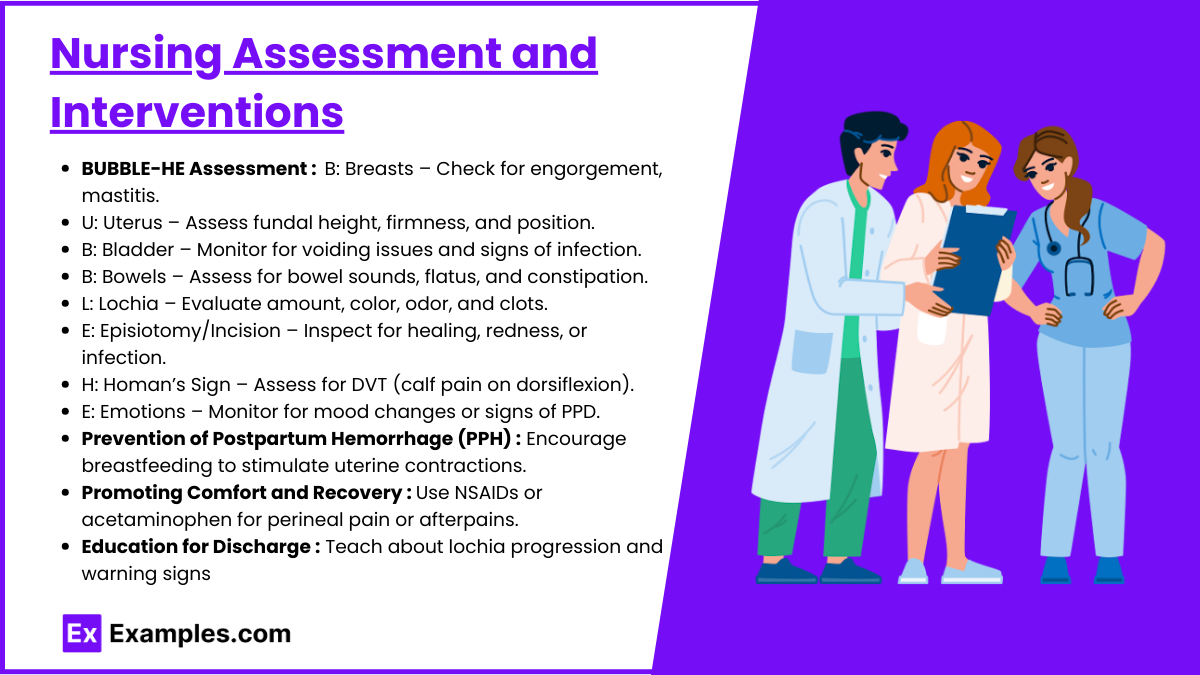
BUBBLE-HE Assessment
- B: Breasts – Check for engorgement, mastitis.
- U: Uterus – Assess fundal height, firmness, and position.
- B: Bladder – Monitor for voiding issues and signs of infection.
- B: Bowels – Assess for bowel sounds, flatus, and constipation.
- L: Lochia – Evaluate amount, color, odor, and clots.
- E: Episiotomy/Incision – Inspect for healing, redness, or infection.
- H: Homan’s Sign – Assess for DVT (calf pain on dorsiflexion).
- E: Emotions – Monitor for mood changes or signs of PPD.
Prevention of Postpartum Hemorrhage (PPH)
- Encourage breastfeeding to stimulate uterine contractions.
- Administer oxytocin if needed to promote uterine tone.
- Massage the uterus if boggy.
Promoting Comfort and Recovery
- Pain Management: Use NSAIDs or acetaminophen for perineal pain or afterpains.
- Perineal Care: Use ice packs, sitz baths, and proper hygiene.
- Ambulation: Early ambulation prevents thrombosis and improves recovery.
Education for Discharge
- Teach about lochia progression and warning signs (e.g., heavy bleeding, foul odor).
- Discuss signs of infection (e.g., fever, chills).
- Provide resources for lactation support and mental health.
Examples
Example 1. Uterine Involution and Fundal Assessment
Postpartum uterine involution is a natural process where the uterus returns to its pre-pregnancy size through contractions and tissue breakdown. Nurses assess the fundus daily, noting its descent approximately 1 cm below the umbilicus per day. A firm, midline fundus is expected; however, a boggy uterus suggests uterine atony and increases the risk of postpartum hemorrhage. Nursing interventions include uterine massage, breastfeeding support to stimulate oxytocin release, and monitoring for heavy bleeding or clots.
Example 2. Lochia Assessment
Lochia, the vaginal discharge following childbirth, undergoes predictable changes in color and quantity. Lochia rubra (bright red) lasts 1–3 days, lochia serosa (pink-brown) lasts 4–10 days, and lochia alba (whitish-yellow) persists for up to 6 weeks. Nurses monitor lochia for abnormal findings, such as heavy bleeding, foul odor, or large clots, which may indicate infection or retained placental fragments. Proper education on lochia progression and signs of complications helps mothers recognize when to seek medical care.
Example 3. Breastfeeding and Nipple Care
Breastfeeding mothers often experience engorgement as milk production begins around postpartum days 3–5. Nurses encourage frequent breastfeeding to relieve engorgement and prevent complications like mastitis. Proper latch techniques are critical to prevent nipple trauma, assessed by observing for redness, cracks, or pain. For non-breastfeeding mothers, supportive measures include wearing a tight-fitting bra, applying cold packs, and avoiding nipple stimulation to suppress lactation.
Example 4. Postpartum Emotional Adjustments
Emotional well-being is a key focus in postpartum care. Mothers may experience postpartum blues, characterized by mood swings, tearfulness, and mild anxiety, resolving within 1–2 weeks. However, persistent sadness, withdrawal, or harmful thoughts signal postpartum depression (PPD), requiring immediate medical intervention. Nurses use screening tools like the Edinburgh Postnatal Depression Scale (EPDS) to identify at-risk mothers and provide emotional support or referrals to mental health professionals.
Example 5. Prevention of Postpartum Hemorrhage (PPH)
Postpartum hemorrhage is a significant concern, defined as blood loss exceeding 500 mL after vaginal birth or 1,000 mL after cesarean delivery. Risk factors include uterine atony, retained placenta, or birth trauma. Nurses prevent PPH by encouraging breastfeeding to stimulate uterine contractions, administering oxytocin as prescribed, and performing uterine massage when the fundus feels boggy. Monitoring vital signs and blood loss ensures timely identification and intervention for hemorrhage.
Practice Questions
Question 1
A nurse is assessing a postpartum patient 24 hours after a vaginal delivery. The patient reports her vaginal bleeding is bright red and saturates a perineal pad every hour. What is the nurse’s priority action?
A. Encourage the patient to breastfeed to promote uterine contractions.
B. Perform fundal massage to ensure the uterus is firm.
C. Increase the patient’s fluid intake to prevent dehydration.
D. Document the findings and reassess in 1 hour.
Answer: B. Perform fundal massage to ensure the uterus is firm.
Explanation:
- Postpartum hemorrhage (PPH) is characterized by excessive bleeding, often caused by uterine atony (failure of the uterus to contract effectively).
- Fundal massage is the immediate intervention to stimulate uterine contractions and reduce bleeding.
- Encouraging breastfeeding (A) can also promote uterine contractions but is not the priority during active hemorrhage.
- Increasing fluids (C) may address fluid loss but does not stop the bleeding.
- Waiting to reassess (D) delays critical care and can lead to worsening hemorrhage.
Question 2
A nurse is caring for a breastfeeding mother who reports severe pain in her left breast and flu-like symptoms. Upon assessment, the nurse notes the breast is red, warm, and tender to touch. What should the nurse do first?
A. Teach the patient to wean the baby to prevent further complications.
B. Administer prescribed antibiotics and pain relievers.
C. Encourage frequent breastfeeding or pumping from the affected breast.
D. Apply cold compresses to the breast to reduce inflammation.
Answer: C. Encourage frequent breastfeeding or pumping from the affected breast.
Explanation:
- The patient is showing signs of mastitis, a common postpartum complication caused by milk stasis or infection (often Staphylococcus aureus).
- Frequent breastfeeding or pumping helps to relieve milk stasis, which is a contributing factor to mastitis.
- Antibiotics (B) are essential but will not immediately relieve milk stasis.
- Weaning (A) is not recommended as it can worsen milk stasis.
- Cold compresses (D) may provide comfort but do not address the underlying issue.
Question 3
A postpartum patient is in the “Taking-Hold” phase. Which statement by the patient indicates this phase of maternal role adaptation?
A. “I can’t stop crying, and I feel overwhelmed by everything.”
B. “Can you show me how to change my baby’s diaper again?”
C. “I just want to rest right now and process the birth.”
D. “I’m starting to feel more comfortable with my role as a mother.”
Answer: B. “Can you show me how to change my baby’s diaper again?”
Explanation:
- The Taking-Hold Phase occurs 2–3 days postpartum and is marked by an increased focus on learning and assuming responsibility for infant care.
- Asking for help with a task like diaper changing reflects eagerness to learn and improve caregiving skills.
- Persistent crying and feeling overwhelmed (A) are characteristic of postpartum blues.
- Wanting to rest and process the birth (C) reflects the Taking-In Phase, which occurs in the first 24–48 hours postpartum.
- Feeling comfortable with motherhood (D) is part of the Letting-Go Phase, which occurs later.