Critical care prioritization is a fundamental skill tested on the NCLEX RN® exam, focusing on the ability to address life-threatening situations efficiently. Nurses must determine which patient needs immediate intervention using frameworks like ABCs (Airway, Breathing, Circulation) and Maslow’s Hierarchy of Needs. This prioritization ensures safety, prevents complications, and saves lives. Understanding acute versus chronic conditions, stable versus unstable patients, and safety risks are crucial for success. Mastery of these principles prepares candidates to make critical decisions confidently, improving patient outcomes and achieving excellence on the NCLEX RN®.
Learning Objectives
In studying “Critical Care: Prioritization” for the NCLEX RN® exam, you should learn to evaluate patient needs using frameworks like ABCs (Airway, Breathing, Circulation) and Maslow’s Hierarchy of Needs. Understand how to differentiate between acute and chronic conditions, and stable versus unstable patients. Analyze safety risks and prioritize interventions based on severity and urgency. Apply principles of the nursing process to assess, plan, implement, and evaluate care. Explore the role of delegation and critical thinking in managing multiple patients. Use this knowledge to interpret and respond effectively to prioritization scenarios in NCLEX-style questions, ensuring optimal patient outcomes.
Prioritization
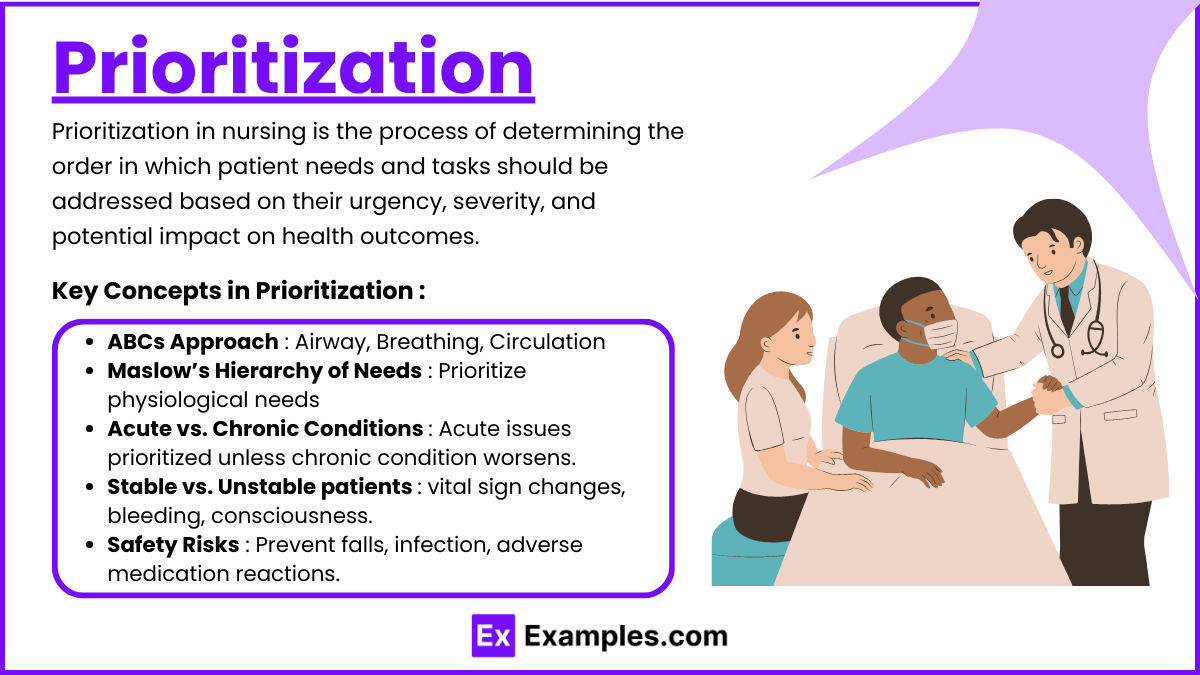
Prioritization in nursing is the process of determining the order in which patient needs and tasks should be addressed based on their urgency, severity, and potential impact on health outcomes. It involves assessing critical factors, such as airway, breathing, circulation (ABCs), and safety risks, to focus on interventions that prevent harm and ensure optimal patient care. Effective prioritization enables nurses to allocate resources and time efficiently, addressing life-threatening issues first while balancing the demands of multiple patients or competing tasks. This skill is fundamental in critical care and is essential for safe, evidence-based nursing practice.
Key Concepts in Prioritization
- ABCs Approach
- Airway: Always assess and secure the airway first. Conditions like obstructions or aspiration take precedence.
- Breathing: Evaluate respiratory rate, oxygen saturation, and ventilatory support. Conditions like pneumothorax or respiratory distress require immediate intervention.
- Circulation: Monitor heart rate, blood pressure, and perfusion. Issues like hemorrhage or cardiac arrest are urgent.
- Maslow’s Hierarchy of Needs
- Prioritize physiological needs (e.g., oxygenation, hydration) over psychological needs (e.g., emotional support).
- Acute vs. Chronic Conditions
- Acute issues often take precedence over chronic conditions unless the chronic condition exacerbates.
- Stable vs. Unstable Patients
- Focus on unstable patients first. Unstable conditions include fluctuating vital signs, active bleeding, or deteriorating consciousness.
- Safety Risks
- Address risks that could lead to immediate harm, such as falls, infection, or adverse medication reactions.
Strategies for Effective Prioritization

Prioritization in nursing is about deciding which tasks, interventions, or patient needs to address first to ensure safety and effective care. For the NCLEX RN® exam, understanding prioritization is crucial for answering critical thinking questions. Below are effective strategies to master prioritization:
- Apply the Nursing Process : The nursing process—Assessment, Diagnosis, Planning, Implementation, and Evaluation (ADPIE)—is the backbone of clinical decision-making.
- Assessment: Collect comprehensive data on patients. Accurate assessment helps identify critical issues.
- Diagnosis: Identify which problems are life-threatening or could worsen quickly.
- Planning: Develop a plan based on immediate needs, addressing life-threatening issues first.
- Implementation: Execute the interventions in the order of priority.
- Evaluation: Reassess outcomes and adjust the plan if the patient’s condition changes.
- Utilize Maslow’s Hierarchy of Needs : Maslow’s model prioritizes physiological needs over psychological or self-fulfillment needs. Focus on life-sustaining interventions first.
- Physiological Needs: Address issues such as oxygen, food, water, and pain relief before emotional support or education.
- Prioritize Acute Over Chronic Conditions : Acute issues that arise suddenly or are life-threatening take precedence over stable chronic conditions.
- Acute: Conditions like sepsis, stroke, or active bleeding need immediate intervention.
- Chronic: Conditions like diabetes or arthritis, while important, can often be addressed later unless they are exacerbated.
- Consider Time-Sensitive Tasks : Interventions that must occur within a specific timeframe should be prioritized.
- Examples:
- Administering medications such as thrombolytics for stroke within the critical time window.
- Monitoring a post-op patient closely during the first hour for signs of complications.
- Delegate Wisely : Delegating tasks effectively helps manage workload and ensures that critical actions are taken promptly. However, tasks involving assessment, teaching, and critical decision-making should not be delegated.
- Example: Assign a CNA to measure vital signs for stable patients while focusing on interventions for an unstable patient yourself.
Tips for NCLEX Success in Prioritization
- Use the ABCs Framework : Always address Airway, Breathing, and Circulation first when determining the priority of care. For example, a patient with difficulty breathing is addressed before one with a non-life-threatening condition.
- Apply Maslow’s Hierarchy of Needs : Prioritize physiological needs such as oxygenation, hydration, and elimination over psychological or self-esteem needs.
- Distinguish Between Acute and Chronic Issues : Acute conditions requiring immediate intervention are prioritized over stable, chronic conditions, even if they are significant.
- Evaluate Patient Stability : Patients with rapidly deteriorating conditions or fluctuating vital signs take precedence over those with stable or improving conditions.
- Focus on Life-Threatening Conditions : Identify and act on conditions that pose an immediate risk to life, such as airway obstruction, cardiac arrest, or severe bleeding.
- Time Management : Allocate adequate time to analyze prioritization questions, but avoid overthinking. Quickly eliminate distractors and focus on the core problem.
Examples
Example 1: Airway Obstruction vs. Pain Management
A nurse is assigned to four patients: one experiencing an airway obstruction with stridor, another requesting pain medication for post-operative discomfort, a third requiring a dressing change, and a fourth waiting for discharge instructions. The priority is the patient with an airway obstruction, as it is life-threatening. Issues involving airway compromise always take precedence over other needs, even if they involve severe pain or routine care tasks.
Example 2: Respiratory Distress vs. Emotional Support
A patient in respiratory distress with labored breathing and oxygen saturation dropping to 88% must be prioritized over a patient expressing anxiety about their diagnosis. Although emotional support is important, it does not outweigh the physiological need for adequate oxygenation. Interventions such as administering oxygen or adjusting ventilator settings are critical to stabilizing the distressed patient before attending to others.
Example 3: Hemorrhage vs. Low-Grade Fever
A patient with post-surgical signs of active hemorrhage (e.g., tachycardia, hypotension, and visible blood loss) takes priority over a patient with a low-grade fever of 100.8°F. Hemorrhage indicates an unstable condition with immediate life-threatening implications, requiring interventions like fluid resuscitation, blood transfusion, or surgical review. The low-grade fever, while requiring attention, does not pose an immediate danger.
Example 4: Unstable Cardiac Rhythm vs. Stable Hypertension
A patient with a new onset of ventricular tachycardia, displaying dizziness and hypotension, requires urgent intervention to prevent cardiac arrest. This patient is prioritized over another with chronic, stable hypertension controlled with medications. Unstable cardiac rhythms are emergencies, demanding rapid monitoring, medication administration, or defibrillation, depending on the severity.
Example 5: Sepsis Management vs. Routine Medication Administration
A patient showing early signs of sepsis—fever, increased heart rate, and low blood pressure—takes precedence over a patient due for their routine morning medications. Sepsis is a systemic, life-threatening condition that requires immediate actions such as initiating IV fluids, obtaining cultures, and administering broad-spectrum antibiotics to prevent progression to septic shock.
Practice Questions
Question 1
A nurse is assigned to care for four patients. Based on prioritization principles, which patient should the nurse attend to first?
A. A 45-year-old with stable vital signs awaiting discharge instructions.
B. A 50-year-old complaining of severe chest pain and diaphoresis.
C. A 60-year-old diabetic requesting a snack due to feeling hungry.
D. A 40-year-old post-op patient requesting assistance to the bathroom.
Answer: B
Explanation:
- Severe chest pain and diaphoresis (B) indicate a potential myocardial infarction (heart attack), which is a life-threatening condition requiring immediate intervention. This aligns with the ABCs framework (Airway, Breathing, Circulation).
- Option A: A stable patient awaiting discharge is a low priority since there is no immediate risk.
- Option C: Hunger in a diabetic patient is important but not an emergency compared to a potential cardiac event.
- Option D: Post-op assistance is routine care and does not take precedence over a life-threatening condition.
Question 2
The nurse enters a room to find a patient gasping for air and clutching their throat, a patient with a 101°F fever requesting water, a post-op patient with a dressing soaked in blood, and a patient complaining of nausea. What is the nurse’s priority?
A. The patient gasping for air.
B. The patient with a 101°F fever.
C. The post-op patient with a bloody dressing.
D. The patient complaining of nausea.
Answer: A
Explanation:
- The patient gasping for air (A) is at immediate risk due to an airway obstruction. According to the ABCs framework, airway is always the first priority.
- Option B: A fever requires attention but is not life-threatening.
- Option C: While a bloody dressing suggests hemorrhage, it is not as critical as airway compromise.
- Option D: Nausea is uncomfortable but not a life-threatening condition.
Question 3
Which task should the nurse delegate to an experienced unlicensed assistive personnel (UAP) while attending to a patient experiencing respiratory distress?
A. Assess the patient’s respiratory rate.
B. Perform a complete bed bath for another patient.
C. Administer a bronchodilator via nebulizer.
D. Provide discharge education to a stable patient.
Answer: B
Explanation:
- Option B: Performing a bed bath is within the scope of practice for a UAP and can be delegated. This allows the nurse to focus on the patient in respiratory distress.
- Option A: Assessment requires nursing judgment and cannot be delegated.
- Option C: Administering medications, including bronchodilators, is a nursing responsibility and cannot be assigned to a UAP.
- Option D: Discharge education requires nursing expertise and critical thinking.