Psychiatric medications are essential in the treatment and management of mental health disorders. For the NCLEX-RN®, it is crucial to understand the different classes of these medications, their mechanisms of action, therapeutic uses, side effects, and nursing considerations. These drugs help stabilize mood, reduce anxiety, manage psychotic symptoms, and improve focus in conditions like depression, anxiety, bipolar disorder, and schizophrenia. Nurses must be prepared to recognize adverse effects, educate patients on medication adherence, and ensure safe administration as part of holistic mental health care.
Learning Objectives
In studying “Mental Health: Psychiatric Medications” for the NCLEX-RN® exam, you should learn to understand the classification, mechanisms of action, and therapeutic uses of key psychiatric medications, including antidepressants, antipsychotics, anxiolytics, mood stabilizers, and stimulants. Analyze how these medications manage mental health disorders like depression, anxiety, bipolar disorder, and schizophrenia. Evaluate the principles behind medication side effects, contraindications, and nursing considerations. Additionally, explore how nurses support safe medication administration, patient education, and monitoring for adverse reactions. Apply this knowledge to interpreting patient care scenarios and answering NCLEX-style questions related to pharmacological interventions in mental health nursing practice.
Overview of Psychiatric Medications
Psychiatric medications are pharmacological agents used to manage, treat, and alleviate the symptoms of various mental health disorders. These medications aim to restore the chemical balance in the brain, improve emotional well-being, and support individuals in leading a more stable and functional life. While psychiatric medications are not considered “cures,” they play a significant role in symptom control and relapse prevention. The prescription of these medications is typically done by psychiatrists, primary care physicians, or other licensed medical professionals.The main classes include:
- Antidepressants : Antidepressants are primarily used to treat depression, but they are also effective for anxiety disorders, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), and other mood-related conditions. These medications work by balancing neurotransmitters like serotonin, norepinephrine, and dopamine.
- Types of Antidepressants:
- Selective Serotonin Reuptake Inhibitors (SSRIs): Examples include fluoxetine, sertraline, and citalopram. These increase serotonin levels in the brain.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Examples include venlafaxine and duloxetine, which boost both serotonin and norepinephrine.
- Tricyclic Antidepressants (TCAs): These older antidepressants, such as amitriptyline and nortriptyline, affect multiple neurotransmitters.
- Monoamine Oxidase Inhibitors (MAOIs): MAOIs like phenelzine and tranylcypromine are used less frequently due to their interaction with certain foods and medications.
- Atypical Antidepressants: Medications like bupropion and mirtazapine do not fit into the above categories but still effectively treat depression.
- Antipsychotics : Antipsychotic medications are used to treat psychotic disorders like schizophrenia, bipolar disorder, and severe depression with psychotic features. They help in managing symptoms such as hallucinations, delusions, and disorganized thinking.
- Types of Antipsychotics:
- First-Generation Antipsychotics (Typical Antipsychotics): Examples include haloperidol and chlorpromazine. These target dopamine receptors to reduce psychotic symptoms.
- Second-Generation Antipsychotics (Atypical Antipsychotics): Examples include olanzapine, risperidone, and aripiprazole. These medications influence both dopamine and serotonin levels.
- Mood Stabilizers : Mood stabilizers are used to treat bipolar disorder and mood swings associated with other mental health disorders. They work by balancing the electrical activity in brain cells and stabilizing mood shifts between mania and depression.
- Types of Mood Stabilizers:
- Lithium: The most well-known mood stabilizer, often considered the “gold standard” for bipolar disorder.
- Anticonvulsants: Originally developed for epilepsy, these include medications like valproic acid, carbamazepine, and lamotrigine, which are now widely used for bipolar disorder.
- Anxiolytics : Anxiolytics, also called anti-anxiety medications, are used to treat anxiety disorders, panic attacks, and insomnia. They reduce overactivity in the central nervous system, promoting a sense of calm and relaxation.
- Types of Anxiolytics:
- Benzodiazepines: Short-term medications for acute anxiety and panic attacks, such as diazepam, lorazepam, and clonazepam.
- Non-Benzodiazepine Anxiolytics: Buspirone, which has a lower risk of dependency compared to benzodiazepines.
- Antihistamines: Sometimes prescribed off-label for anxiety (like hydroxyzine).
- Stimulants : Stimulants are used to treat attention-deficit/hyperactivity disorder (ADHD) and narcolepsy. They increase the activity of dopamine and norepinephrine in the brain, which helps with attention, focus, and impulse control.
- Types of Stimulants:
- Amphetamines: Medications like Adderall (amphetamine/dextroamphetamine) and Vyvanse (lisdexamfetamine).
- Methylphenidate: Includes drugs like Ritalin and Concerta, which affect dopamine and norepinephrine.
Therapeutic Uses, Side Effects, and Monitoring
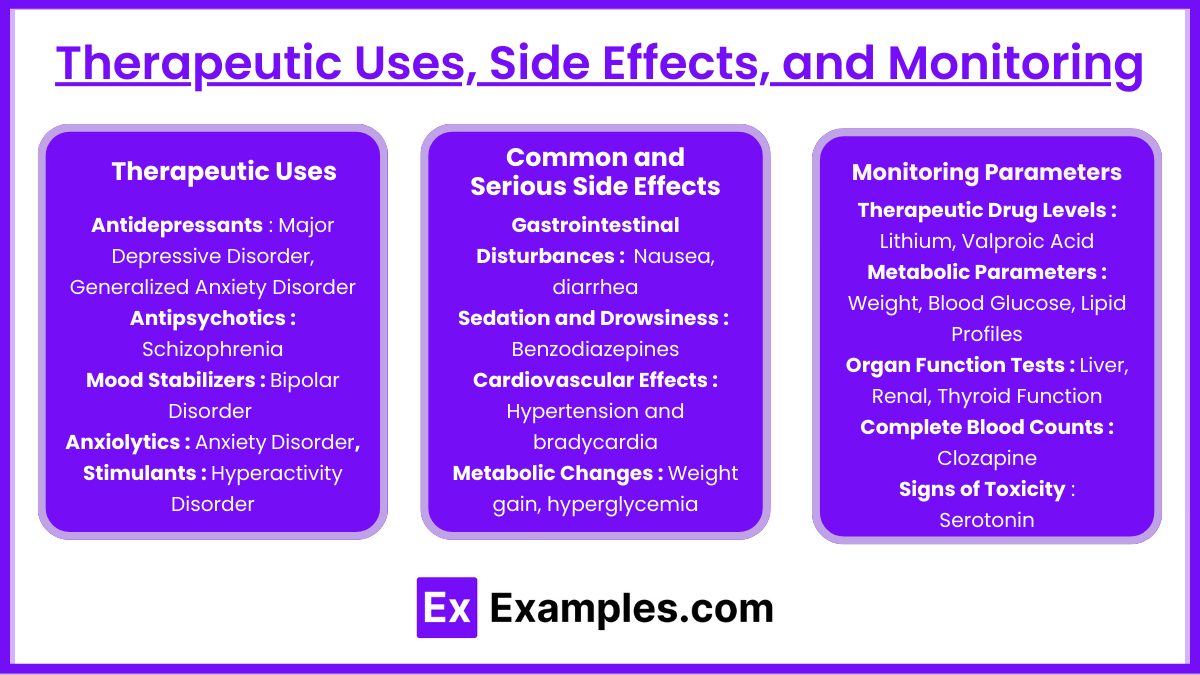
This section delves into the specific indications for each medication class, common and severe side effects, and essential monitoring parameters to ensure safe and effective patient care.
Therapeutic Uses
1. Antidepressants
- Primary Uses: Major Depressive Disorder, Generalized Anxiety Disorder, Panic Disorder, Obsessive-Compulsive Disorder (OCD), Post-Traumatic Stress Disorder (PTSD)
- Additional Uses: Chronic pain, certain eating disorders
2. Antipsychotics
- Primary Uses: Schizophrenia, Acute psychotic episodes, Bipolar Disorder (manic phases)
- Additional Uses: Tourette’s syndrome, severe behavioral problems in children, augmenting antidepressants in major depressive disorder
3. Mood Stabilizers
- Primary Uses: Bipolar Disorder (both manic and depressive episodes), Preventing mood swings
- Additional Uses: Augmentation in treatment-resistant depression
4. Anxiolytics
- Primary Uses: Generalized Anxiety Disorder, Panic Attacks, Acute anxiety relief, Seizure disorders (benzodiazepines)
- Additional Uses: Muscle relaxation, alcohol withdrawal management
5. Stimulants
- Primary Uses: Attention-Deficit/Hyperactivity Disorder (ADHD), Narcolepsy
- Additional Uses: Treatment-resistant depression (sometimes)
Common and Serious Side Effects
1. Gastrointestinal Disturbances
- SSRIs/SNRIs: Nausea, diarrhea
- TCAs: Constipation, dry mouth
2. Sedation and Drowsiness
- Antipsychotics (First and Second-Gen), Benzodiazepines, Trazodone: Can impair alertness and daily functioning
3. Cardiovascular Effects
- SNRIs: Hypertension
- Antipsychotics (First-Gen): Orthostatic hypotension
- Clonidine: Hypotension, bradycardia
4. Metabolic Changes
- Second-Generation Antipsychotics: Weight gain, hyperglycemia, dyslipidemia
- Mood Stabilizers (Lithium, Valproic Acid): Weight gain, thyroid dysfunction (Lithium)
5. Neurological Effects
- Lithium: Tremors, ataxia
- Benzodiazepines/Stimulants: Tics, seizures (especially with Bupropion at high doses)
Monitoring Parameters
1. Therapeutic Drug Levels
- Lithium: 0.6-1.2 mEq/L (toxicity >1.5 mEq/L)
- Valproic Acid: 50-100 µg/mL
- Carbamazepine: Therapeutic range varies (typically 4-12 µg/mL)
- Clozapine: Regular CBCs (weekly initially, then biweekly after 6 months)
2. Metabolic Parameters
- Weight, Blood Glucose, Lipid Profiles: Particularly with second-generation antipsychotics
3. Organ Function Tests
- Liver Function: Valproic Acid, Carbamazepine
- Renal Function: Lithium
- Thyroid Function: Lithium (risk of hypothyroidism)
4. Complete Blood Counts (CBC)
- Clozapine: To monitor for agranulocytosis
5. Signs of Toxicity and Adverse Reactions
- Lithium Toxicity: Nausea, vomiting, tremors, confusion
- Serotonin Syndrome: Agitation, hyperreflexia, tremors
- NMS: Fever, muscle rigidity
- Tardive Dyskinesia: Involuntary facial movements
Examples
Example 1: Sertraline
Sertraline, a Selective Serotonin Reuptake Inhibitor (SSRI), is commonly prescribed for the treatment of major depressive disorder (MDD), anxiety disorders, post-traumatic stress disorder (PTSD), and obsessive-compulsive disorder (OCD). It works by increasing serotonin levels in the brain, thereby improving mood, reducing anxiety, and alleviating symptoms of depression. When preparing for the NCLEX-RN®, it is crucial to understand the key nursing considerations, including monitoring for signs of suicidal ideation (especially in adolescents and young adults), assessing for serotonin syndrome (manifested by confusion, fever, and muscle rigidity), and advising patients to avoid abrupt discontinuation due to withdrawal effects. Patient education also includes avoiding the use of St. John’s Wort, as it can increase the risk of serotonin syndrome.
Example 2: Haloperidol
Haloperidol is a first-generation (typical) antipsychotic used to manage schizophrenia, acute psychosis, and Tourette syndrome. It works by blocking dopamine receptors in the brain, thereby reducing symptoms such as hallucinations, delusions, and disorganized thinking. For NCLEX-RN® preparation, nurses must be aware of its most significant side effect — extrapyramidal symptoms (EPS) — which can manifest as tardive dyskinesia (involuntary movements), dystonia (muscle spasms), and akathisia (restlessness). Nurses should also monitor for signs of neuroleptic malignant syndrome (NMS), a life-threatening condition characterized by fever, muscle rigidity, and altered mental status. Interventions include stopping the medication and providing supportive care. Patient education involves explaining the importance of adhering to the prescribed dosage and attending follow-up appointments for monitoring of side effects.
Example 3: Lithium
Lithium is a classic mood stabilizer used to treat bipolar disorder, particularly in managing manic episodes. It works by modulating neurotransmitters and stabilizing the electrical activity in brain cells. On the NCLEX-RN®, test-takers should recognize the importance of therapeutic drug monitoring, as the therapeutic range of lithium is 0.6 to 1.2 mEq/L, with levels above 1.5 mEq/L considered toxic. Signs of lithium toxicity include nausea, vomiting, diarrhea, tremors, and confusion. Patients should be advised to maintain consistent fluid and sodium intake to avoid fluctuations in lithium levels. Nursing care involves regular monitoring of renal function and thyroid function, as lithium can affect these systems over time. Patient education should emphasize the importance of hydration and the need to report symptoms of toxicity immediately.
Example 4: Lorazepam
Lorazepam, a benzodiazepine, is prescribed for anxiety, panic disorders, and acute agitation. It enhances the action of gamma-aminobutyric acid (GABA), a neurotransmitter that induces a calming effect. From an NCLEX-RN® perspective, the most crucial nursing consideration is the risk of dependence and withdrawal, especially with long-term use. Nurses should administer this medication cautiously in patients with a history of substance use disorder. Additionally, respiratory depression is a key concern, particularly in elderly patients or those receiving opioids or CNS depressants. Nurses should ensure that patients avoid alcohol while taking lorazepam. For acute overdose, the antidote flumazenil can be administered. Patient education includes taking the medication exactly as prescribed and not stopping it abruptly to avoid withdrawal symptoms like insomnia, tremors, and seizures.
Example 5: Methylphenidate
Methylphenidate, commonly known as Ritalin, is a stimulant used to treat attention-deficit/hyperactivity disorder (ADHD) and narcolepsy. It increases the activity of dopamine and norepinephrine, which improves focus, attention, and impulse control. For NCLEX-RN® test preparation, nurses must know that this drug can lead to insomnia, loss of appetite, weight loss, and tachycardia. Nursing care involves monitoring weight and tracking growth in pediatric patients, as stimulants can suppress appetite and impact growth. Parents should be instructed to administer the medication in the morning to prevent sleep disturbances. Nurses should also educate patients and caregivers about the risk of misuse and the need for proper storage, as stimulants have a high potential for abuse.
Practice Questions
Question 1
A nurse is caring for a client who has been prescribed fluoxetine (Prozac) for major depressive disorder. Which of the following client statements indicates a need for further teaching?
A. “I will avoid taking St. John’s Wort while on this medication.”
B. “It may take several weeks before I start feeling better.”
C. “I can stop taking this medication as soon as I feel better.”
D. “I might experience mild nausea when I first start taking this medication.”
Answer: C
Explanation: Option C is the correct answer because it indicates a misunderstanding of proper medication adherence. Fluoxetine (Prozac) is a Selective Serotonin Reuptake Inhibitor (SSRI), and sudden discontinuation can lead to withdrawal symptoms such as dizziness, irritability, anxiety, and mood disturbances. Patients should be instructed to continue taking the medication as prescribed, even after they start feeling better. Discontinuation should be gradual and under the guidance of a healthcare provider.
- Option A: This is a correct understanding. St. John’s Wort can increase serotonin levels and, when combined with fluoxetine, may cause serotonin syndrome, a potentially life-threatening condition.
- Option B: This is also correct. Antidepressants like fluoxetine typically take 4 to 6 weeks before their full therapeutic effects are noticed.
- Option D: This is another correct statement. Mild gastrointestinal side effects such as nausea and diarrhea are common in the early weeks of taking an SSRI.
Question 2
A nurse is monitoring a client who has been taking lithium for the treatment of bipolar disorder. Which of the following assessment findings should be the nurse’s priority to report to the healthcare provider?
A. Mild hand tremors
B. Serum lithium level of 1.2 mEq/L
C. Persistent diarrhea and vomiting
D. Increased thirst and frequent urination
Answer: C
Explanation: Option C is the correct answer because persistent diarrhea and vomiting can lead to dehydration, which increases the risk of lithium toxicity. Lithium has a narrow therapeutic index (0.6–1.2 mEq/L) and is excreted through the kidneys. Loss of fluids (through diarrhea or vomiting) reduces renal clearance, causing an increase in serum lithium levels, leading to toxicity. Symptoms of lithium toxicity include confusion, ataxia, tremors, and severe gastrointestinal disturbances.
- Option A: Mild hand tremors are a common side effect of lithium and do not necessarily indicate toxicity. However, coarse tremors are a sign of toxicity.
- Option B: A serum lithium level of 1.2 mEq/L is at the upper end of the therapeutic range but is not toxic. However, close monitoring is required if it approaches 1.5 mEq/L.
- Option D: Increased thirst and frequent urination (polyuria) are side effects of lithium due to its effect on the kidneys (nephrogenic diabetes insipidus). While concerning, it is not as critical as signs of lithium toxicity like persistent vomiting or diarrhea.
Question 3
A client with generalized anxiety disorder (GAD) has been prescribed lorazepam (Ativan). Which of the following is the most important teaching point for the nurse to discuss with the client?
A. “Take this medication only when you feel extremely anxious.”
B. “Avoid driving or operating heavy machinery while taking this medication.”
C. “This medication has a low risk of addiction or dependence.”
D. “You can safely consume small amounts of alcohol while taking this medication.”
Answer: B
Explanation: Option B is the correct answer because lorazepam (Ativan) is a benzodiazepine, which causes sedation, drowsiness, and impaired motor coordination. Patients taking benzodiazepines should avoid activities that require full attention, such as driving or operating heavy machinery, due to the risk of accidents.
- Option A: While some benzodiazepines may be prescribed on an “as-needed” (PRN) basis, lorazepam is often used on a regular schedule for generalized anxiety disorder (GAD) to prevent breakthrough anxiety. The method of administration is individualized to the patient.
- Option C: This is incorrect. Benzodiazepines are habit-forming and have a high potential for dependence and tolerance. Clients must be educated about the potential for abuse and withdrawal symptoms.
- Option D: This is incorrect. Combining benzodiazepines with alcohol can result in severe respiratory depression, sedation, and even death. Clients should be taught to avoid alcohol and other central nervous system (CNS) depressants.