Pharmacology of psychiatric medications is a crucial component for the NCLEX-RN® exam, encompassing a wide range of drugs used to manage mental health disorders. This field includes antidepressants, antipsychotics, mood stabilizers, anxiolytics, and stimulants, each with specific mechanisms, indications, and side effects. Understanding these medications enables nurses to administer treatments safely, monitor patient responses, and provide effective education. Mastery of psychiatric pharmacology is essential for delivering compassionate, evidence-based care to individuals with mental health needs.
Learning Objectives
In studying “Pharmacology: Psychiatric Medications” for the NCLEX-RN® Exam, you should learn to understand the various classes of psychiatric drugs, including antidepressants, antipsychotics, mood stabilizers, anxiolytics, and stimulants. Analyze the mechanisms of action, therapeutic indications, and common side effects associated with each medication class. Evaluate nursing considerations such as patient monitoring, potential drug interactions, and safety precautions. Additionally, explore the clinical applications of these medications in treating mental health disorders and managing patient care, and apply your understanding to effectively respond to pharmacology-related scenarios and questions on the NCLEX-RN® exam.
Types of Psychiatric Medications
Psychiatric medications, also known as psychotropic medications, are a class of drugs designed to manage and alleviate symptoms associated with various mental health disorders. These medications work by altering the chemical balance in the brain, influencing neurotransmitters such as serotonin, dopamine, norepinephrine, and gamma-aminobutyric acid (GABA). The primary goal of psychiatric medications is to improve mood, cognition, behavior, and overall functioning in individuals with psychiatric conditions.
- Antidepressants
- Antipsychotics
- Mood Stabilizers
- Anxiolytics
Antidepressants
Antidepressants are medications used to treat major depressive disorder and other conditions like anxiety disorders, OCD, and PTSD. They work by altering neurotransmitter levels in the brain.
1.Selective Serotonin Reuptake Inhibitors (SSRIs)
- Examples: Fluoxetine (Prozac), Sertraline (Zoloft), Citalopram (Celexa), Escitalopram (Lexapro), Paroxetine (Paxil)
- Mechanism of Action: Inhibit the reuptake of serotonin in the brain, increasing serotonin levels.
- Indications: Depression, anxiety disorders, OCD, PTSD, panic disorder.
- Common Side Effects: Nausea, insomnia, sexual dysfunction, headache, gastrointestinal disturbances.
- Nursing Considerations:
- Monitor for serotonin syndrome (symptoms: confusion, rapid heart rate, high blood pressure, dilated pupils, loss of muscle coordination).
- Advise patients to report suicidal thoughts, especially in young adults.
- Educate about gradual onset of therapeutic effects (2-4 weeks).
- Patient Teaching:
- Take consistently at the same time each day.
- Do not discontinue abruptly to avoid withdrawal symptoms.
2. Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- Examples: Venlafaxine (Effexor), Duloxetine (Cymbalta), Desvenlafaxine (Pristiq)
- Mechanism of Action: Inhibit the reuptake of both serotonin and norepinephrine.
- Indications: Depression, anxiety disorders, neuropathic pain.
- Common Side Effects: Hypertension, nausea, dizziness, dry mouth, insomnia.
- Nursing Considerations:
- Monitor blood pressure regularly.
- Assess for signs of hypertension.
- Patient Teaching:
- Report any increase in blood pressure.
- Avoid abrupt discontinuation.
3. Tricyclic Antidepressants (TCAs)
- Examples: Amitriptyline, Nortriptyline (Pamelor), Imipramine (Tofranil), Desipramine (Norpramin)
- Mechanism of Action: Block the reuptake of norepinephrine and serotonin; also affect other neurotransmitters.
- Indications: Depression, certain anxiety disorders, chronic pain.
- Common Side Effects: Dry mouth, constipation, urinary retention, blurred vision, sedation, orthostatic hypotension, weight gain.
- Nursing Considerations:
- Monitor cardiovascular status (risk of arrhythmias, especially in overdose).
- Caution in patients with glaucoma or urinary retention.
- Patient Teaching:
- Rise slowly from sitting or lying positions to prevent dizziness.
- Avoid alcohol as it can enhance sedation.
4. Monoamine Oxidase Inhibitors (MAOIs)
- Examples: Phenelzine (Nardil), Tranylcypromine (Parnate), Isocarboxazid (Marplan)
- Mechanism of Action: Inhibit monoamine oxidase, preventing the breakdown of neurotransmitters like serotonin, norepinephrine, and dopamine.
- Indications: Depression, atypical depression, Parkinson’s disease adjunct.
- Common Side Effects: Orthostatic hypotension, weight gain, sexual dysfunction, insomnia, dizziness.
- Nursing Considerations:
- Dietary Restrictions: Avoid tyramine-rich foods (e.g., aged cheeses, cured meats, soy products) to prevent hypertensive crisis.
- Monitor blood pressure regularly.
- Patient Teaching:
- Strictly adhere to dietary restrictions.
- Report any severe headaches or chest pain immediately.
Antipsychotics
Antipsychotics are used to manage symptoms of psychosis, such as those found in schizophrenia and bipolar disorder. They work by altering dopamine and serotonin neurotransmission. they are two types of Antipsychotics.
1. First-Generation (Typical) Antipsychotics
- Examples: Haloperidol (Haldol), Chlorpromazine (Thorazine), Fluphenazine (Prolixin)
- Mechanism of Action: Dopamine D2 receptor antagonists, primarily blocking dopamine pathways.
- Indications: Schizophrenia, acute psychotic episodes, mania.
- Common Side Effects: Extrapyramidal symptoms (EPS) such as dystonia, akathisia, parkinsonism, tardive dyskinesia; sedation; hypotension; anticholinergic effects.
- Nursing Considerations:
- Monitor for EPS and tardive dyskinesia.
- Assess for signs of neuroleptic malignant syndrome (fever, muscle rigidity, altered mental status).
- Patient Teaching:
- Report any uncontrolled movements or stiffness.
- Adherence to medication to prevent relapse.
2. Second-Generation (Atypical) Antipsychotics
- Examples: Risperidone (Risperdal), Olanzapine (Zyprexa), Quetiapine (Seroquel), Aripiprazole (Abilify), Clozapine (Clozaril)
- Mechanism of Action: Block dopamine and serotonin receptors; fewer EPS compared to typical antipsychotics.
- Indications: Schizophrenia, bipolar disorder, adjunct in depression, irritability in autism.
- Common Side Effects: Weight gain, metabolic syndrome (hyperglycemia, dyslipidemia), sedation, extrapyramidal symptoms (less common), agranulocytosis (Clozapine).
- Nursing Considerations:
- Monitor blood glucose and lipid levels.
- Regularly assess weight and BMI.
- Clozapine requires regular CBC monitoring due to risk of agranulocytosis.
- Patient Teaching:
- Maintain a balanced diet and exercise to manage weight gain.
- Report signs of infection (especially with Clozapine).
- Adhere to regular laboratory testing schedules.
Mood Stabilizers
Mood Stabilizers are a class of psychiatric medications used primarily to regulate and stabilize mood swings in individuals diagnosed with mood disorders, particularly bipolar disorder. These medications help prevent the recurrence of manic and depressive episodes, promoting mood stability and enhancing the patient’s ability to function effectively in daily life. Used primarily in bipolar disorder to stabilize mood swings between mania and depression.
1. Lithium
- Mechanism of Action: Modulates neurotransmitter release, alters second messenger systems, neuroprotective effects.
- Indications: Bipolar disorder (manic and maintenance phases), augmentation in depression.
- Common Side Effects: Tremors, polyuria, polydipsia, hypothyroidism, weight gain, gastrointestinal upset, renal impairment.
- Nursing Considerations:
- Monitor serum lithium levels (therapeutic range: 0.6-1.2 mEq/L).
- Monitor kidney and thyroid function.
- Ensure adequate hydration to prevent toxicity.
- Patient Teaching:
- Report signs of lithium toxicity (tremors, confusion, ataxia, seizures).
- Maintain consistent salt and fluid intake.
- Do not discontinue abruptly.
2. Anticonvulsants as Mood Stabilizers
- Examples: Valproic acid (Depakote), Lamotrigine (Lamictal), Carbamazepine (Tegretol), Oxcarbazepine (Trileptal)
- Mechanism of Action: Varies by drug; generally modulate neurotransmitter release, stabilize neuronal membranes.
- Indications: Bipolar disorder, seizures, migraine prophylaxis.
- Common Side Effects:
- Valproic Acid: GI upset, hepatotoxicity, thrombocytopenia, weight gain, tremors.
- Lamotrigine: Rash (potentially Stevens-Johnson syndrome), dizziness, headache.
- Carbamazepine: Dizziness, hyponatremia, agranulocytosis, rash.
- Nursing Considerations:
- Regularly monitor liver function tests (Valproic acid).
- Monitor for signs of rash (Lamotrigine).
- Monitor CBC and sodium levels (Carbamazepine).
- Patient Teaching:
- Report any unusual rashes or signs of infection.
- Adhere to prescribed dosing schedule to maintain therapeutic levels.
- Avoid abrupt discontinuation to prevent seizures or mood destabilization.
Anxiolytics
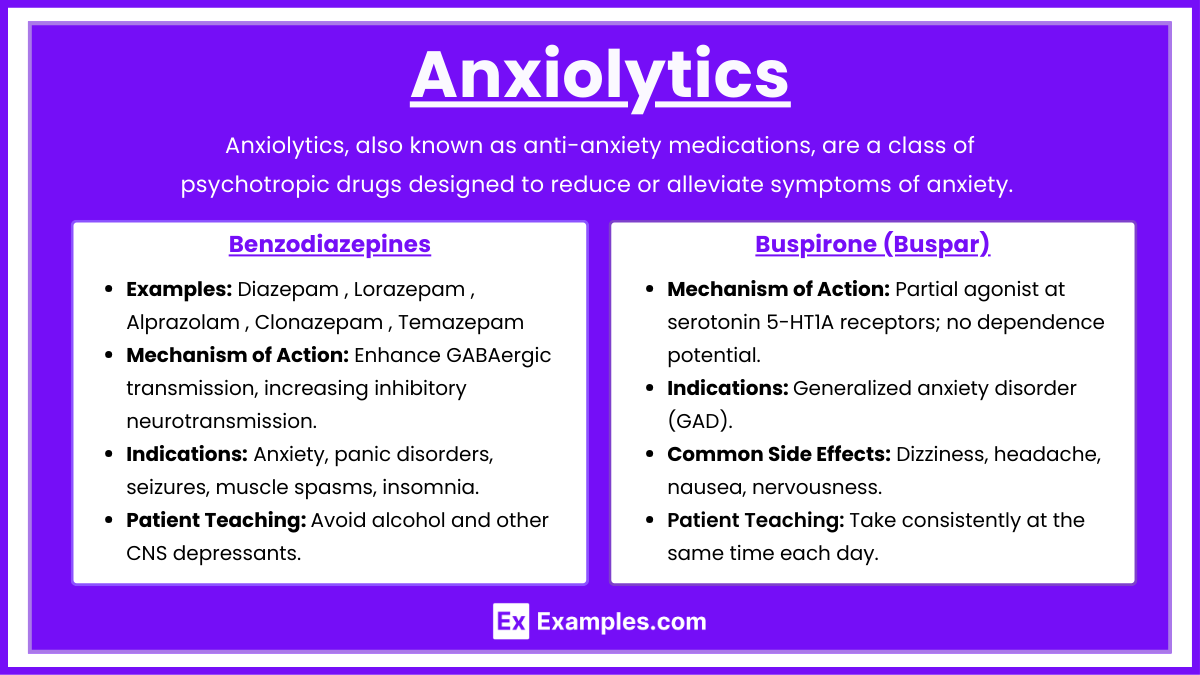
Anxiolytics, also known as anti-anxiety medications, are a class of psychotropic drugs designed to reduce or alleviate symptoms of anxiety. These medications work by targeting various neurotransmitter systems in the brain to produce a calming effect, thereby helping individuals manage excessive fear, worry, and agitation associated with anxiety disorders. Used to manage anxiety disorders, panic attacks, and sometimes insomnia.
1. Benzodiazepines
- Examples: Diazepam (Valium), Lorazepam (Ativan), Alprazolam (Xanax), Clonazepam (Klonopin), Temazepam (Restoril)
- Mechanism of Action: Enhance GABAergic transmission, increasing inhibitory neurotransmission.
- Indications: Anxiety, panic disorders, seizures, muscle spasms, insomnia (short-term).
- Common Side Effects: Drowsiness, dizziness, confusion, ataxia, respiratory depression (with high doses or in combination with other CNS depressants).
- Nursing Considerations:
- Assess for risk of dependence and abuse.
- Use the lowest effective dose for the shortest duration possible.
- Monitor for signs of sedation and respiratory depression.
- Patient Teaching:
- Avoid alcohol and other CNS depressants.
- Do not drive or operate heavy machinery until alert.
- Do not discontinue abruptly to prevent withdrawal symptoms.
2. Buspirone (Buspar)
- Mechanism of Action: Partial agonist at serotonin 5-HT1A receptors; no dependence potential.
- Indications: Generalized anxiety disorder (GAD).
- Common Side Effects: Dizziness, headache, nausea, nervousness.
- Nursing Considerations:
- Takes several weeks to achieve therapeutic effect.
- Less sedating; may be preferred for long-term management.
- Patient Teaching:
- Take consistently at the same time each day.
- Do not expect immediate relief of anxiety symptoms.
Examples
Example 1. Fluoxetine (Prozac) – Selective Serotonin Reuptake Inhibitor (SSRI)
Fluoxetine is a widely used antidepressant from the SSRI class. It treats major depressive disorder (MDD), anxiety, panic disorder, and obsessive-compulsive disorder (OCD). It works by inhibiting the reuptake of serotonin in the brain, increasing serotonin availability to improve mood. For the NCLEX RN®, it is essential to remember that common side effects include nausea, weight gain, insomnia, and sexual dysfunction. Nursing considerations include monitoring for signs of serotonin syndrome (confusion, agitation, rapid heart rate) and advising patients not to stop the medication abruptly. Patients should also be educated about potential interactions with other serotonin-enhancing medications like MAOIs and St. John’s wort, as these can increase the risk of serotonin syndrome.
Example 2. Haloperidol (Haldol) – Typical Antipsychotic
Haloperidol is a first-generation (typical) antipsychotic used primarily to treat schizophrenia, acute psychosis, and severe agitation. It works by blocking dopamine D2 receptors in the brain, thereby reducing psychotic symptoms like hallucinations and delusions. A major NCLEX RN® focus is on extrapyramidal symptoms (EPS) such as dystonia (muscle spasms), akathisia (restlessness), and tardive dyskinesia (involuntary facial movements). Neuroleptic malignant syndrome (NMS) is a severe but rare side effect characterized by high fever, altered mental status, and muscle rigidity. Nursing considerations include frequent monitoring for signs of EPS, encouraging hydration, and avoiding the abrupt discontinuation of the drug. Patients should be educated to avoid alcohol while on Haloperidol.
Example 3. Lithium – Mood Stabilizer
Lithium is a gold-standard treatment for bipolar disorder and is one of the most important mood stabilizers to master for the NCLEX RN®. Lithium works by affecting sodium transport in nerve and muscle cells, stabilizing mood swings in patients with bipolar disorder. The therapeutic range for lithium is 0.6 to 1.2 mEq/L, and it requires close monitoring to prevent toxicity. Signs of lithium toxicity include nausea, vomiting, diarrhea, confusion, tremors, and seizures. NCLEX RN® test-takers must know that dehydration, low sodium levels, and the use of diuretics increase the risk of lithium toxicity. Nursing considerations include advising patients to maintain consistent fluid and salt intake and to avoid nonsteroidal anti-inflammatory drugs (NSAIDs) that may increase lithium levels. Routine blood work is required to monitor the drug’s therapeutic level.
Example 4. Lorazepam (Ativan) – Benzodiazepine
Lorazepam is an anxiolytic (anti-anxiety) drug from the benzodiazepine class. It is commonly used to treat anxiety, panic attacks, and insomnia, as well as for sedation before medical procedures. Lorazepam works by enhancing the activity of GABA, a calming neurotransmitter, producing a sedative, hypnotic, and anxiolytic effect. The NCLEX RN® exam often asks about its potential for abuse, dependency, and withdrawal symptoms, as well as the risk of respiratory depression. Nursing considerations include advising patients to avoid alcohol, avoid operating heavy machinery, and not to stop the medication abruptly. Lorazepam is also used for status epilepticus, a medical emergency. For this reason, nurses should monitor the patient’s respiratory rate, level of sedation, and blood pressure when administering the drug.
Example 5. Clozapine (Clozaril) – Atypical Antipsychotic
Clozapine is an atypical (second-generation) antipsychotic used to treat treatment-resistant schizophrenia. Unlike typical antipsychotics, it targets both dopamine and serotonin receptors, improving both positive symptoms (like hallucinations) and negative symptoms (like social withdrawal). For the NCLEX RN®, a key focus is agranulocytosis, a life-threatening drop in white blood cell count. Nurses must monitor white blood cell (WBC) counts weekly for the first six months and bi-weekly thereafter. Side effects like drowsiness, dizziness, weight gain, and hypersalivation are common, but agranulocytosis is the most critical to identify. Patients taking clozapine should be educated about the importance of regular blood tests and instructed to report any signs of infection, such as sore throat or fever, as these could be signs of agranulocytosis.
Practice Questions
Question 1
A patient with bipolar disorder is being treated with lithium. Which of the following signs should the nurse monitor for as an indication of lithium toxicity?
A) Bradycardia
B) Diarrhea
C) Tremors
D) Hypercalcemia
Answer: C) Tremors
Explanation : Tremors: One of the earliest and most common signs of lithium toxicity. Patients may experience fine hand tremors that worsen with intention. Other Signs: Nausea, vomiting, diarrhea, ataxia, confusion, and in severe cases, seizures or coma.
Why the Other Options Are Incorrect:
- A) Bradycardia: Lithium toxicity is more commonly associated with cardiac conduction delays, such as sinoatrial node dysfunction leading to various arrhythmias, but bradycardia is not a primary indicator.
- B) Diarrhea: While gastrointestinal disturbances like diarrhea can occur with lithium toxicity, tremors are more specific and prominent.
- D) Hypercalcemia: Lithium can affect calcium metabolism, potentially causing hypercalcemia, but tremors are a more immediate and recognizable sign of toxicity.
Question 2
A patient is prescribed sertraline (Zoloft) for major depressive disorder. Which of the following patient statements indicates a need for further teaching?
A) “I might experience some nausea when I start this medication.”
B) “I should avoid taking this medication with alcohol.”
C) “It’s important to take this medication every day, even if I feel better.”
D) “I can stop taking this medication as soon as my symptoms improve.”
Answer: D) “I can stop taking this medication as soon as my symptoms improve.
Explanation : ” Understanding SSRIs and Patient Education: SSRIs (e.g., Sertraline): These medications typically take 2-4 weeks to exhibit therapeutic effects. Patients must continue taking them even after feeling better to prevent relapse.
Why the Other Options Are Correct Statements:
- A) Nausea: Common side effect when initiating SSRIs; patients should be aware and manage accordingly.
- B) Alcohol Avoidance: Alcohol can exacerbate depression and counteract the benefits of SSRIs; it’s advisable to avoid or limit alcohol intake.
- C) Daily Adherence: Consistent daily intake maintains steady medication levels, essential for effectiveness.
Why Option D Is Incorrect:
- Stopping Medication Early: Abruptly discontinuing SSRIs can lead to withdrawal symptoms and potential relapse of depression. Patients should be advised to consult their healthcare provider before making any changes to their medication regimen.
Question 3:
A patient diagnosed with schizophrenia has been prescribed risperidone (Risperdal). Which laboratory test should the nurse ensure is conducted regularly due to a serious potential side effect of this medication?
A) Complete blood count (CBC)
B) Fasting blood glucose
C) Lipid profile
D) Prolactin levels
Answer: A) Complete blood count (CBC)
Explanation : Risperidone (Risperdal): While risperidone is a second-generation antipsychotic and generally has a lower risk of extrapyramidal symptoms compared to first-generation antipsychotics, it can still cause agranulocytosis, a potentially life-threatening drop in white blood cells. CBC Monitoring: Regular CBCs help in early detection of agranulocytosis, allowing for timely intervention.
Why the Other Options Are Less Critical for Risperidone:
- B) Fasting Blood Glucose: While second-generation antipsychotics can affect glucose metabolism, risperidone is less notorious for causing hyperglycemia compared to others like olanzapine.
- C) Lipid Profile: Risperidone may have some impact on lipid levels, but this is not as immediate or critical as the risk for agranulocytosis.
- D) Prolactin Levels: Risperidone can increase prolactin levels, leading to side effects like galactorrhea or gynecomastia, but routine CBC is more crucial due to the severity of agranulocytosis.