The respiratory system plays a critical role in maintaining oxygenation and removing carbon dioxide, essential for cellular function. For the NCLEX-RN®, understanding respiratory disorders like asthma, COPD, pneumonia, and pulmonary embolism is vital for effective patient care. These conditions often require prompt interventions, emphasizing airway management, oxygenation, and critical thinking skills. Nurses must be adept at assessing respiratory symptoms, interpreting diagnostic tests, and prioritizing interventions using the ABC framework. Mastering respiratory nursing ensures optimal outcomes and is a cornerstone of NCLEX success.
Learning Objectives
In studying “Respiratory” for the NCLEX-RN® Exam, you should learn to assess, diagnose, and manage respiratory disorders such as asthma, COPD, pneumonia, and pulmonary embolism. Understand key interventions like oxygen therapy, bronchodilators, and mechanical ventilation to address airway and breathing issues. Evaluate diagnostic tools such as ABGs, pulmonary function tests, and chest X-rays to interpret patient conditions. Additionally, analyze prioritization strategies using the ABCs framework and apply knowledge to clinical scenarios. Explore how these interventions and assessments are used to manage respiratory emergencies and chronic conditions, ensuring safe and effective patient care in NCLEX practice questions.
Introduction of Respiratory
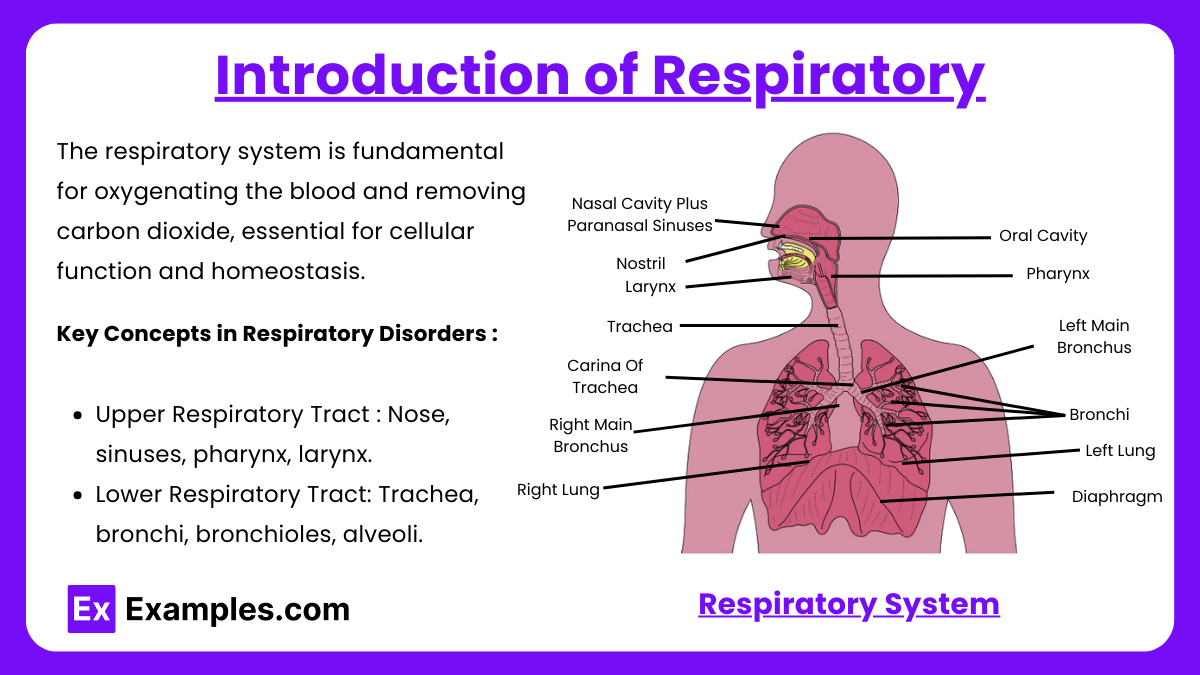
The respiratory system is fundamental for oxygenating the blood and removing carbon dioxide, essential for cellular function and homeostasis. For the NCLEX-RN®, understanding the respiratory system’s anatomy, physiology, and clinical applications ensures readiness for questions focused on conditions like asthma, COPD, and pneumonia. The NCLEX tests your ability to assess, diagnose, and manage these conditions while applying critical thinking skills for patient prioritization and interventions.
Key Concepts in Respiratory Disorders
1. Anatomy and Physiology
- Upper Respiratory Tract: Nose, sinuses, pharynx, larynx.
- Lower Respiratory Tract: Trachea, bronchi, bronchioles, alveoli.
- Gas Exchange: Occurs in the alveoli; requires proper ventilation and perfusion (V/Q matching).
- Accessory Muscles: Intercostal muscles and diaphragm assist breathing.
2. Respiratory Assessment
- Subjective Data: Dyspnea, orthopnea, chest pain, cough (productive or non-productive), hemoptysis.
- Objective Data:
- Auscultation: Crackles (fluid), wheezes (bronchoconstriction), stridor (obstruction).
- Respiratory Rate and Pattern: Tachypnea, bradypnea, Cheyne-Stokes.
- Oximetry: Normal SpO₂ is 95%-100%; hypoxemia if <90%.
- Arterial Blood Gases (ABGs):
- pH: 7.35-7.45
- PaCO₂: 35-45 mmHg
- PaO₂: 80-100 mmHg
- HCO₃⁻: 22-26 mEq/L
Common Respiratory Disorders
- Asthma: A chronic inflammatory condition causing airway hyperresponsiveness, wheezing, and coughing. Management includes bronchodilators (albuterol) for acute attacks and corticosteroids for long-term control.
- Chronic Obstructive Pulmonary Disease (COPD): Includes emphysema and chronic bronchitis, presenting with dyspnea, productive cough, and fatigue. Management focuses on bronchodilators, smoking cessation, and oxygen therapy.
- Pneumonia: Infection of the lungs leading to fever, chills, and productive cough. Treatment includes antibiotics, hydration, and incentive spirometry.
- Pulmonary Embolism (PE): A life-threatening blockage in the pulmonary artery. Symptoms include sudden dyspnea and chest pain. Anticoagulation therapy is the primary treatment.
- Acute Respiratory Distress Syndrome (ARDS): Severe alveolar damage resulting in hypoxemia unresponsive to oxygen therapy. Requires mechanical ventilation and addressing the underlying cause.
These disorders demand precise assessment and intervention, including patient education, medication management, and diagnostic tools like ABGs and imaging studies.
Prioritization in Respiratory Conditions (NCLEX Strategy)
The ABCDE framework (Airway, Breathing, Circulation, Disability, Exposure) is the cornerstone for prioritization in respiratory care:
- Airway: Always ensure a clear and patent airway. For patients with obstructions or swelling, interventions may include suctioning, intubation, or positioning.
- Breathing: Assess oxygen saturation, respiratory rate, and effort. Administer oxygen or initiate mechanical ventilation as needed.
- Circulation: Evaluate for signs of hypoperfusion or shock. In conditions like pulmonary embolism, circulatory support is critical.
- Disability: Monitor neurological status as hypoxia can cause altered mental status or confusion.
- Exposure: Identify any external factors contributing to respiratory distress, such as trauma or environmental allergens.
In the NCLEX, prioritize interventions based on life-threatening conditions. For example, hypoxemia in a COPD patient takes precedence over less urgent symptoms like fatigue or sputum production. Understanding this hierarchy is vital for answering prioritization questions correctly.
Examples
Example 1: Asthma Attack
A 45-year-old patient presents with sudden shortness of breath, wheezing, and use of accessory muscles. The nurse prioritizes administering a short-acting beta-agonist (e.g., albuterol) via a metered-dose inhaler or nebulizer. The patient is placed in a high Fowler’s position to improve breathing and oxygenation, and oxygen therapy is initiated if SpO₂ drops below 90%. Patient education includes trigger avoidance and proper inhaler use to prevent future exacerbations.
Example 2: Chronic Obstructive Pulmonary Disease (COPD) Exacerbation
A 68-year-old patient with COPD arrives with dyspnea, chronic productive cough, and cyanosis. The nurse prioritizes maintaining oxygen saturation between 88%-92% using low-flow oxygen (to prevent CO₂ retention). Bronchodilators, corticosteroids, and antibiotics (if infection is present) are administered as prescribed. The NCLEX may also assess the nurse’s ability to educate the patient on smoking cessation and pulmonary rehabilitation.
Example 3: Pneumonia in an Elderly Patient
A 72-year-old patient is admitted with fever, crackles on auscultation, pleuritic chest pain, and a productive cough with purulent sputum. The nurse collects a sputum culture before administering prescribed antibiotics, monitors oxygenation, and encourages the use of an incentive spirometer to prevent atelectasis. Nursing interventions focus on hydration and repositioning to improve lung expansion and secretion clearance.
Example 4: Pulmonary Embolism (PE)
A 55-year-old postoperative patient suddenly develops sharp chest pain, shortness of breath, and tachycardia. The nurse immediately raises the head of the bed, administers oxygen, and notifies the provider. Diagnostic tests such as D-dimer and CT pulmonary angiography confirm the diagnosis. Treatment involves anticoagulation therapy (e.g., heparin) and monitoring for complications like hypoxemia or shock.
Example 5: Acute Respiratory Distress Syndrome (ARDS)
A 60-year-old patient with sepsis develops severe hypoxemia, refractory to supplemental oxygen. The nurse prioritizes maintaining adequate oxygenation through mechanical ventilation with low tidal volumes to prevent ventilator-induced lung injury. Additional interventions include positioning the patient prone to improve oxygenation and monitoring for hemodynamic stability. The NCLEX may test knowledge on managing ARDS while addressing the underlying cause, such as infection or trauma.
Practice Questions
Question 1
A nurse is caring for a client experiencing an acute asthma attack. The client is wheezing, using accessory muscles to breathe, and has a respiratory rate of 30 breaths per minute. What is the nurse’s priority intervention?
A. Administer albuterol via nebulizer as prescribed.
B. Check oxygen saturation with a pulse oximeter.
C. Encourage the client to take slow, deep breaths.
D. Notify the healthcare provider immediately.
Answer: A. Administer albuterol via nebulizer as prescribed.
Explanation: This client is experiencing bronchospasm, which leads to airway obstruction. Administering a short-acting beta-agonist like albuterol relaxes bronchial smooth muscles, providing immediate relief. Checking oxygen saturation is important but not the first action. Encouraging deep breaths is secondary after alleviating acute symptoms. Notifying the provider is necessary if the condition worsens, but immediate intervention should be prioritized.
Question 2
A client with chronic obstructive pulmonary disease (COPD) reports increased dyspnea. The nurse notes diminished breath sounds and a respiratory rate of 24 breaths per minute. Which action should the nurse take first?
A. Increase the oxygen flow rate to 4 L/min.
B. Place the client in high Fowler’s position.
C. Administer the prescribed bronchodilator.
D. Encourage pursed-lip breathing.
Answer: B. Place the client in high Fowler’s position.
Explanation: High Fowler’s position optimizes lung expansion, improving ventilation and reducing dyspnea. This is the quickest non-invasive intervention. Increasing oxygen flow requires caution in COPD clients to avoid suppressing their respiratory drive. Administering a bronchodilator is appropriate but follows proper positioning. Pursed-lip breathing is beneficial but not the priority intervention.
Question 3
A postoperative client is hesitant to use the incentive spirometer despite instructions. The client reports mild discomfort and fatigue. What is the nurse’s best response?
A. Administer pain medication before using the incentive spirometer.
B. Explain that using the incentive spirometer can prevent complications like pneumonia.
C. Encourage the client to take short walks instead of using the incentive spirometer.
D. Notify the provider about the client’s reluctance to follow instructions.
Answer: B. Explain that using the incentive spirometer can prevent complications like pneumonia.
Explanation: Providing education helps the client understand the importance of the intervention, increasing compliance. Preventing atelectasis and pneumonia is a critical postoperative goal. While administering pain medication can help with spirometer use, it should be paired with education. Short walks promote mobility but do not specifically target lung expansion. Notifying the provider is unnecessary for manageable non-compliance.