Critical care respiratory management is a vital component of nursing practice, particularly for the NCLEX-RN® exam. This topic encompasses life-threatening respiratory conditions such as Acute Respiratory Distress Syndrome (ARDS), pulmonary embolism, respiratory failure, and the use of mechanical ventilation. Nurses must understand the pathophysiology, prioritize interventions, and monitor for complications to ensure patient safety. Proficiency in recognizing early signs of respiratory distress, interpreting ABGs, and managing ventilated patients is essential for delivering optimal care and excelling in the NCLEX-RN®.
Learning Objectives
In studying “Critical Care: Respiratory” for the NCLEX-RN® exam, you should learn to understand the assessment and management of life-threatening respiratory conditions, including Acute Respiratory Distress Syndrome (ARDS), mechanical ventilation, and respiratory failure. Analyze the principles of oxygenation, ventilation, and airway management, along with interventions like prone positioning, suctioning, and pharmacological treatments. Evaluate complications such as ventilator-associated pneumonia and tension pneumothorax. Explore how these concepts apply in clinical scenarios to prioritize patient care and interpret critical respiratory data, including arterial blood gases (ABGs). Apply your understanding to respond to NCLEX-style questions that require critical thinking and prioritization.
Key Respiratory Conditions in Critical Care
Critical care respiratory concepts are fundamental in managing patients with life-threatening respiratory conditions. Understanding respiratory anatomy, pathophysiology, and nursing interventions for conditions like ARDS, mechanical ventilation, and pulmonary emergencies is crucial for NCLEX-RN®. These scenarios test critical thinking and the ability to prioritize interventions effectively.
1. Acute Respiratory Distress Syndrome (ARDS)
- Pathophysiology: ARDS results from direct or indirect injury to the lungs, leading to inflammation and fluid accumulation in the alveoli, impairing oxygen exchange. Common causes include sepsis, trauma, and pneumonia.
- Assessment: Monitor for severe dyspnea, hypoxemia unresponsive to oxygen, and chest X-ray findings showing bilateral infiltrates. Early detection is critical.
- Management: Focus on oxygenation using high-flow oxygen or mechanical ventilation with low tidal volumes and high PEEP. Positioning the patient prone can improve oxygenation.
2. Pulmonary Embolism (PE)
- Pathophysiology: A clot, often from deep vein thrombosis, lodges in pulmonary arteries, obstructing blood flow and gas exchange.
- Key Indicators: Sudden dyspnea, chest pain, tachycardia, hemoptysis, and hypoxia.
- Interventions: Administer anticoagulants like heparin or thrombolytics for massive PE. Position the patient in Fowler’s to facilitate breathing. Use compression devices and encourage ambulation post-surgery to prevent DVT.
3. Respiratory Failure
- Type I (Hypoxemic): Inadequate oxygenation (PaO₂ < 60 mmHg) due to conditions like ARDS or pneumonia.
- Type II (Hypercapnic): CO₂ retention (PaCO₂ > 50 mmHg) often caused by COPD, asthma, or neuromuscular disorders.
- Nursing Role: Immediate oxygen therapy, frequent ABG monitoring, and preparing for potential intubation and mechanical ventilation.
Mechanical Ventilation: Essential Concepts
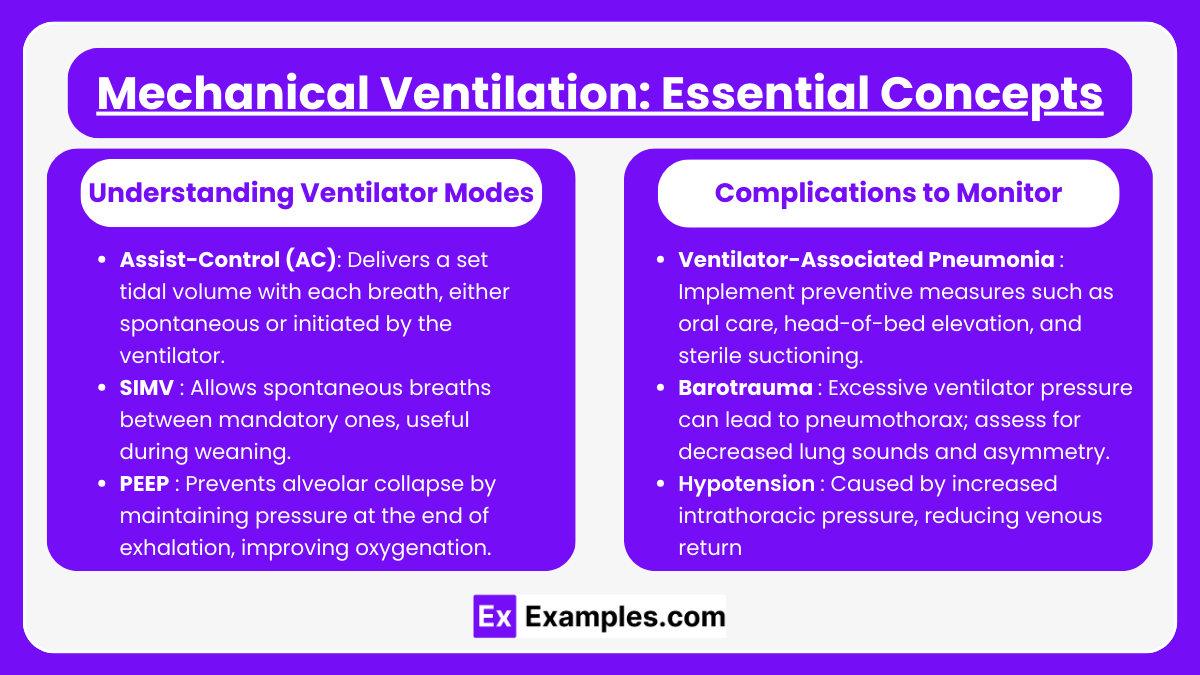
Understanding Ventilator Modes
- Assist-Control (AC): Delivers a set tidal volume with each breath, either spontaneous or initiated by the ventilator. Ideal for resting the respiratory muscles.
- SIMV (Synchronized Intermittent Mandatory Ventilation): Allows spontaneous breaths between mandatory ones, useful during weaning.
- PEEP (Positive End-Expiratory Pressure): Prevents alveolar collapse by maintaining pressure at the end of exhalation, improving oxygenation.
Complications to Monitor
- Ventilator-Associated Pneumonia (VAP): Implement preventive measures such as oral care, head-of-bed elevation, and sterile suctioning.
- Barotrauma: Excessive ventilator pressure can lead to pneumothorax; assess for decreased lung sounds and asymmetry.
- Hypotension: Caused by increased intrathoracic pressure, reducing venous return and cardiac output.
Nursing Interventions for Respiratory Emergencies
- Oxygenation Management : Administer oxygen using the appropriate device: nasal cannula for mild hypoxia, non-rebreather mask for severe cases. Assess the effectiveness of therapy using SpO₂ and ABG levels.
- Airway Management : Ensure the airway is clear by suctioning as needed using sterile technique. For patients with endotracheal tubes or tracheostomies, monitor for signs of obstruction, infection, or dislodgement.
- Pharmacological Interventions : Administer bronchodilators (e.g., albuterol) for bronchospasms and corticosteroids to reduce inflammation. Provide sedatives or neuromuscular blocking agents for patients on ventilators to prevent ventilator asynchrony.
- Monitoring and Diagnostics : Regularly evaluate ABGs to assess oxygenation (PaO₂), ventilation (PaCO₂), and acid-base balance (pH). Use chest X-rays and pulmonary function tests to track progress or detect complications such as pneumothorax or atelectasis.
- Patient Education and Comfort : Educate patients and families about the goals and process of mechanical ventilation. Provide emotional support and manage pain to reduce anxiety and improve cooperation during respiratory care.
Examples
Example 1: Acute Respiratory Distress Syndrome (ARDS)
A life-threatening condition often triggered by sepsis, trauma, or pneumonia. ARDS results in severe inflammation and fluid accumulation in the alveoli, causing hypoxemia unresponsive to oxygen therapy. For NCLEX, expect scenarios emphasizing interventions such as mechanical ventilation with low tidal volume, high PEEP, prone positioning to improve oxygenation, and monitoring for complications like barotrauma or oxygen toxicity.
Example 2: Pulmonary Embolism (PE)
A sudden blockage of pulmonary arteries, typically caused by a thrombus originating in deep veins (DVT). NCLEX questions often describe symptoms like dyspnea, chest pain, and tachycardia, requiring nurses to prioritize anticoagulant administration (e.g., heparin), oxygen therapy, and emergency interventions like thrombolysis for massive PEs. Prevention strategies like early ambulation and the use of compression devices are also critical topics.
Example 3: Tension Pneumothorax
An emergency caused by air trapping in the pleural space, leading to lung collapse and mediastinal shift. Key NCLEX features include hypotension, tracheal deviation, and decreased breath sounds on the affected side. Questions often test your ability to identify this condition quickly and initiate life-saving measures, such as needle decompression followed by chest tube placement.
Example 4: Acute Exacerbation of Chronic Obstructive Pulmonary Disease (COPD)
A worsening of respiratory symptoms in COPD patients, often triggered by infection or environmental factors. NCLEX scenarios may focus on administering bronchodilators (e.g., albuterol), corticosteroids, and oxygen therapy while avoiding excessive oxygen levels to prevent CO₂ retention. Patient education about smoking cessation and pulmonary rehabilitation is also commonly tested.
Example 5: Status Asthmaticus
A severe, prolonged asthma attack unresponsive to standard treatments like bronchodilators. NCLEX questions often describe patients with severe dyspnea, wheezing, or silent chest (indicative of impending respiratory failure). Interventions include high-flow oxygen, systemic corticosteroids, continuous nebulized bronchodilators, and potential intubation for respiratory support. Recognizing early signs of deterioration is critical for managing this condition.
Practice Questions
Question 1
A patient is admitted with Acute Respiratory Distress Syndrome (ARDS). The nurse notes severe hypoxia despite 100% oxygen being administered via a non-rebreather mask. What is the next best nursing intervention?
A. Administer a bronchodilator.
B. Prepare for endotracheal intubation.
C. Increase oxygen flow rate.
D. Place the patient in the supine position.
Answer: B. Prepare for endotracheal intubation.
Explanation:
- ARDS causes impaired gas exchange due to fluid-filled alveoli and decreased lung compliance. If oxygenation is inadequate despite high-flow oxygen, mechanical ventilation is required.
- A: Bronchodilators are used for conditions like asthma or COPD but are not first-line treatment for ARDS.
- C: Increasing the flow rate will not resolve the hypoxia because the underlying issue is impaired alveolar gas exchange.
- D: Supine positioning can worsen oxygenation. Prone positioning is preferred to improve lung ventilation in ARDS.
Question 2
A nurse caring for a mechanically ventilated patient notes diminished breath sounds on the right side, hypotension, and tracheal deviation to the left. What is the nurse’s priority action?
A. Notify the healthcare provider immediately.
B. Suction the endotracheal tube.
C. Increase oxygen delivery on the ventilator.
D. Perform chest physiotherapy on the right side.
Answer: A. Notify the healthcare provider immediately.
Explanation:
- These findings are consistent with tension pneumothorax, a medical emergency caused by air trapping in the pleural space, leading to lung collapse and mediastinal shift.
- Immediate intervention, such as needle decompression or chest tube insertion, is needed to relieve the pressure.
- B: Suctioning addresses airway secretions but will not resolve a tension pneumothorax.
- C: Increasing oxygen does not treat the underlying cause.
- D: Chest physiotherapy is contraindicated in pneumothorax as it can worsen the condition.
Question 3
A patient develops sudden-onset dyspnea, tachycardia, and pleuritic chest pain after surgery. What intervention should the nurse anticipate first?
A. Administer anticoagulation therapy.
B. Perform a CT pulmonary angiography.
C. Apply sequential compression devices (SCDs).
D. Place the patient in Trendelenburg position.
Answer: B. Perform a CT pulmonary angiography.
Explanation:
- The patient’s symptoms suggest a pulmonary embolism (PE). The priority is to confirm the diagnosis with imaging, such as a CT pulmonary angiogram, before initiating treatment.
- A: While anticoagulation therapy is standard for PE treatment, it should not be administered until the diagnosis is confirmed.
- C: SCDs are used to prevent clots but are not appropriate once a PE is suspected.
- D: Trendelenburg position is not beneficial for PE and can worsen the patient’s respiratory status.