Safety and infection control are critical components of the NCLEX RN® exam, emphasizing a nurse’s ability to create and maintain a safe healthcare environment while preventing the spread of infections. These principles are essential for protecting patients, healthcare workers, and visitors from harm. Topics include standard precautions, transmission-based precautions, fall prevention, hazard management, and aseptic techniques. Mastering these concepts not only prepares you for the exam but also equips you with the skills to deliver safe and effective patient care in real-world settings.
Learning Objectives
In studying “Fundamentals: Safety/Infection Control” for the NCLEX RN® exam, you should learn to understand the essential principles of maintaining patient and healthcare worker safety, including standard and transmission-based precautions. Analyze how infection control techniques like hand hygiene, personal protective equipment (PPE), and sterile procedures prevent healthcare-associated infections (HAIs). Evaluate protocols for safe patient handling, fall prevention, and the proper use of restraints. Additionally, explore the role of environmental controls, hazardous material handling, and patient education in ensuring safety. Apply this understanding to assess and manage patient care scenarios, prioritizing interventions and identifying potential risks effectively in NCLEX-style questions.
Infection Control Standards and Protocols
Focus on standard precautions, hand hygiene techniques, and transmission-based precautions, including contact, droplet, and airborne protocols. Understand aseptic techniques and the appropriate use of personal protective equipment (PPE) to prevent infection spread.
- Standard Precautions:
These apply to all patients regardless of their diagnosis or infection status. Always wear gloves when there is potential contact with bodily fluids, and use other PPE as necessary. Hand hygiene before and after patient contact is mandatory. - Transmission-Based Precautions:
Tailored to specific infectious agents to prevent spread:- Contact Precautions: For pathogens like MRSA or C. difficile. Require gloves and gowns. Use dedicated patient equipment.
- Droplet Precautions: For illnesses like influenza or pertussis. Use a surgical mask and maintain spatial separation of at least 3 feet.
- Airborne Precautions: For infections like tuberculosis and chickenpox. Require an N95 respirator and a negative pressure room.
- Hand Hygiene:
The cornerstone of infection control. Wash hands with soap and water for at least 20 seconds, or use an alcohol-based hand rub if hands are not visibly soiled. - Sterile Techniques:
Critical for invasive procedures like catheter insertion or surgical interventions. Maintain sterility by avoiding contamination of sterile fields and using appropriate tools and PPE.
Ensuring Patient Safety
Patient safety is central to nursing care and includes preventing harm through proactive measures.
- Fall Prevention:
Falls are a common source of injury in healthcare settings. Ensure beds are in the lowest position, use non-slip footwear, and implement fall-risk protocols for vulnerable patients. - Restraints:
Use restraints only as a last resort and with a physician’s order. Always choose the least restrictive option, and regularly monitor the patient’s condition and skin integrity. - Patient Identification:
Use two identifiers, such as the patient’s full name and date of birth, before any procedure, medication administration, or treatment. Avoid relying on room numbers or other ambiguous identifiers. - Hazardous Material Handling:
Familiarize yourself with Material Safety Data Sheets (MSDS) for safe handling of chemicals. When working with radiation, use protective gear like lead aprons and follow time-distance-shielding principles to limit exposure. - Environmental Controls:
Disinfect high-touch surfaces regularly, manage waste according to biohazard protocols, and ensure proper ventilation in isolation rooms.
Exam-Specific Strategies for Safety/Infection Control
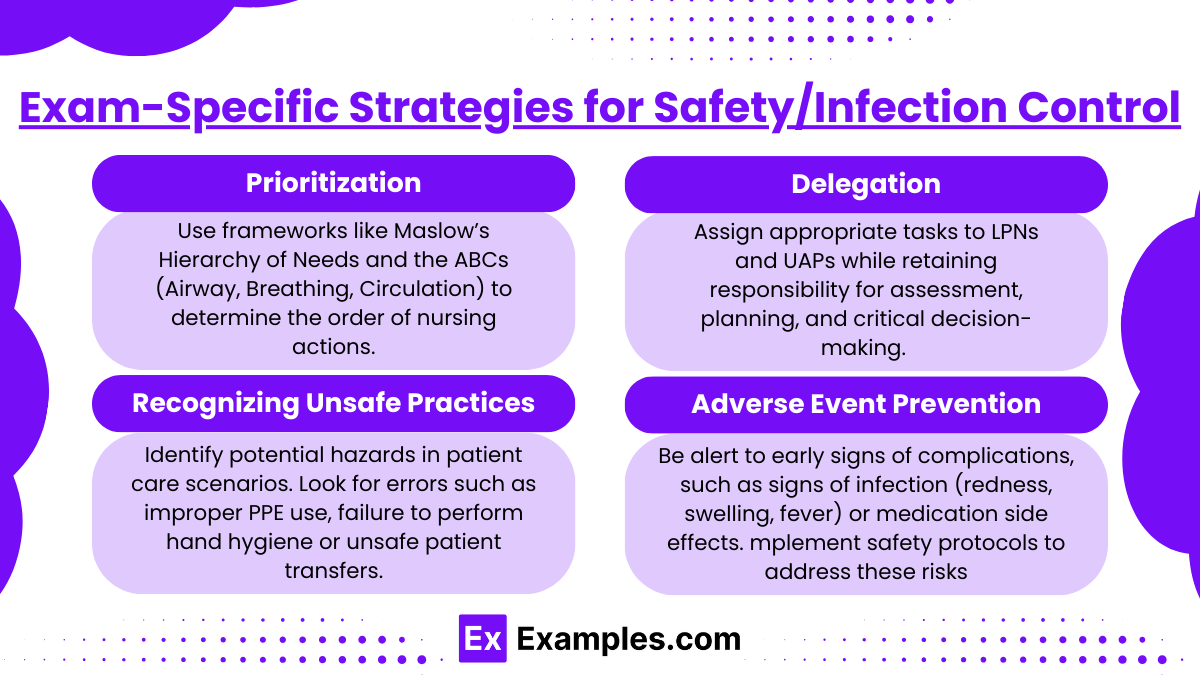
Success on the NCLEX requires not only knowledge but also the ability to apply it effectively in exam scenarios.
- Prioritization:
Use frameworks like Maslow’s Hierarchy of Needs and the ABCs (Airway, Breathing, Circulation) to determine the order of nursing actions. Safety always takes precedence over less critical interventions. - Delegation:
Assign appropriate tasks to LPNs and UAPs while retaining responsibility for assessment, planning, and critical decision-making. For example, an LPN can perform wound care under supervision, but assessing the wound’s condition is the RN’s role. - Recognizing Unsafe Practices:
Identify potential hazards in patient care scenarios. Look for errors such as improper PPE use, failure to perform hand hygiene, or unsafe patient transfers. - Adverse Event Prevention:
Be alert to early signs of complications, such as signs of infection (redness, swelling, fever) or medication side effects. Implement safety protocols to address these risks proactively.
Examples
Example 1: Hand Hygiene Before and After Patient Contact
During a patient interaction, a nurse enters a room and performs hand hygiene using an alcohol-based hand rub. After assisting the patient with personal hygiene, the nurse repeats hand hygiene before leaving the room. This question could test your knowledge of proper hand hygiene protocols and when they should be performed.
Example 2: Implementing Isolation Precautions
A patient is admitted with a diagnosis of tuberculosis. The nurse assigns the patient to a negative-pressure isolation room and ensures all staff wear N95 respirators before entering. The NCLEX could present a scenario asking which precautions are appropriate for specific diseases, requiring you to identify airborne precautions and their implementation.
Example 3: Preventing Patient Falls
A nurse identifies a patient as a high fall risk due to impaired mobility and recent surgery. The nurse implements fall prevention strategies, such as lowering the bed, applying non-slip socks, placing the call light within reach, and ensuring a bedside commode is available. A related NCLEX question might assess your ability to identify effective interventions to reduce the risk of patient falls.
Example 4: Safe Use of Restraints
A nurse cares for a patient who is disoriented and attempting to pull out their IV line. After obtaining a physician’s order, the nurse applies a soft wrist restraint, ensuring that it is not too tight and checking the patient’s skin integrity and circulation every two hours. The NCLEX might include a scenario asking you to choose the correct procedure for using restraints and ensuring patient safety.
Example 5: Handling Sharps and Biohazardous Waste
While administering an injection, a nurse safely disposes of the used needle in a designated sharps container without recapping it. Additionally, the nurse places contaminated dressings in a biohazard bag for disposal. The NCLEX could test your knowledge of proper sharps handling and biohazard disposal procedures to prevent injuries and infections.
Practice Questions
Question 1
A nurse is preparing to care for a patient with Clostridioides difficile (C. difficile). Which of the following infection control measures should the nurse implement?
A. Wear an N95 respirator when entering the room
B. Perform hand hygiene using alcohol-based hand sanitizer after patient care
C. Use gloves and a gown when providing care
D. Place the patient in a room with positive pressure ventilation
Answer: C. Use gloves and a gown when providing care
Explanation: Correct. C. difficile requires contact precautions, which include gloves and gowns to prevent the spread of spores.
- A. Wear an N95 respirator when entering the room: Incorrect. N95 respirators are used for airborne precautions, such as with tuberculosis, not for contact precautions required for C. difficile.
- B. Perform hand hygiene using alcohol-based hand sanitizer after patient care: Incorrect. Alcohol-based sanitizers are not effective against C. difficile spores; soap and water must be used.
- D. Place the patient in a room with positive pressure ventilation: Incorrect. Positive pressure rooms are used for patients needing protection from external contaminants, not for controlling contact-spread pathogens.
Question 2
A nurse is caring for a patient who has been placed on droplet precautions. Which of the following personal protective equipment (PPE) is required when entering the patient’s room?
A. N95 respirator and gloves
B. Surgical mask
C. Gloves and gown only
D. Face shield and gown
Answer: B. Surgical mask
Explanation: Correct B. Droplet precautions are used for diseases like influenza, which require wearing a surgical mask within 3 feet of the patient to prevent transmission via large droplets.
- A. N95 respirator and gloves: Incorrect. An N95 respirator is required for airborne precautions, not droplet precautions.
- C. Gloves and gown only: Incorrect. Gloves and gowns are insufficient for droplet precautions, as a mask is specifically needed to protect against droplet spread.
- D. Face shield and gown: Incorrect. A face shield may be necessary if there is a risk of splashing, but it is not the primary requirement for droplet precautions.
Question 3
The nurse is teaching a newly hired nursing assistant about handling biohazardous waste. Which statement by the nursing assistant indicates the need for further teaching?
A. “I should place used needles in a puncture-proof sharps container.”
B. “Contaminated dressings should be disposed of in a biohazard bag.”
C. “It’s okay to recap needles if I’m careful.”
D. “I should wear gloves when handling soiled linen.”
Answer: C. “It’s okay to recap needles if I’m careful.”
Explanation:
- A. “I should place used needles in a puncture-proof sharps container.”: Correct. Used needles must always be disposed of in a sharps container to prevent needlestick injuries.
- B. “Contaminated dressings should be disposed of in a biohazard bag.”: Correct. Dressings contaminated with bodily fluids are considered biohazardous waste.
- C. “It’s okay to recap needles if I’m careful.”: Incorrect. Recapping needles increases the risk of accidental needlestick injuries and is not recommended. The CDC advises against recapping needles in standard practice.
- D. “I should wear gloves when handling soiled linen.”: Correct. Gloves are necessary to prevent contact with potentially infectious materials in soiled linens.