The Fundamentals: Skills/Procedures section of the NCLEX-RN® exam assesses your ability to perform essential nursing tasks with precision and care. This includes mastering core skills like infection control, medication administration, and patient safety measures. It tests your ability to prioritize, adapt, and respond effectively to clinical scenarios, ensuring patient well-being. A solid grasp of these fundamental procedures is crucial, as they form the foundation of nursing practice. Excelling in this area demonstrates competence in delivering safe and effective patient care.
Learning Objectives
In studying "Fundamentals: Skills/Procedures" for the NCLEX-RN® exam, you should learn to master the foundational nursing skills essential for safe and effective patient care. Understand techniques such as infection control, vital signs assessment, medication administration, and wound care. Analyze the principles of procedures like catheterization, oxygen therapy, and pain management. Evaluate strategies for ensuring patient safety, including fall prevention, proper use of restraints, and maintaining asepsis. Additionally, explore how these skills apply in diverse clinical settings, prioritize patient needs, and practice interpreting scenarios to identify the most appropriate interventions, enhancing your readiness for NCLEX practice questions and real-world nursing.
Key Topics in Skills/Procedures
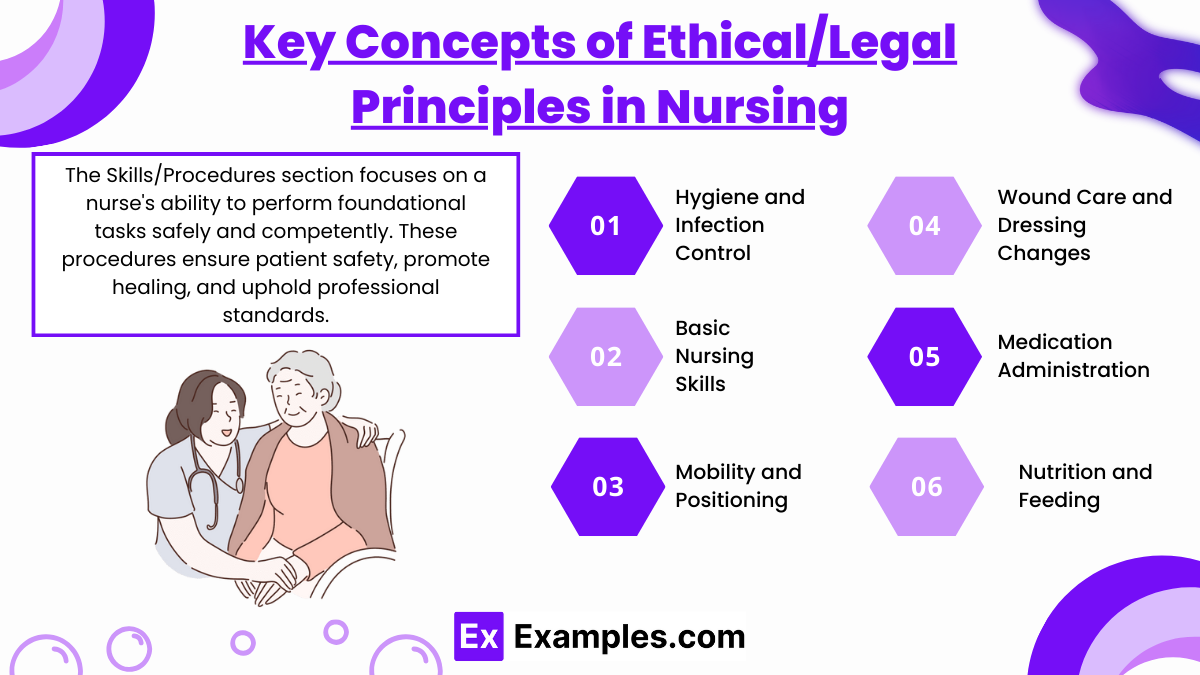
The Skills/Procedures section focuses on a nurse's ability to perform foundational tasks safely and competently. These procedures ensure patient safety, promote healing, and uphold professional standards. Key skills include hygiene, mobility, wound care, and medication administration. Understanding the rationale behind each skill and adhering to evidence-based practices is essential for NCLEX-RN® success.
1. Hygiene and Infection Control
Proper hand hygiene techniques (handwashing and alcohol-based rubs).
Application of personal protective equipment (PPE) based on transmission-based precautions.
Sterile and aseptic technique during procedures like catheter insertion and dressing changes.
2. Basic Nursing Skills
Vital Signs Measurement:
Techniques for measuring blood pressure, temperature, pulse, and respiration.
Interpretation of abnormal values and their implications.
Oxygenation and Airway Management:
Administration of oxygen via nasal cannula, face masks, or Venturi systems.
Suctioning techniques (oropharyngeal and tracheal).
Use of incentive spirometry to promote lung expansion.
3. Mobility and Positioning
Techniques for turning, transferring, and ambulating patients.
Use of assistive devices (walkers, crutches, wheelchairs).
Prevention of complications like pressure ulcers through proper positioning.
4. Wound Care and Dressing Changes
Types of dressings (dry, wet-to-dry, hydrocolloid).
Cleaning techniques for wounds, including irrigation.
Staging and management of pressure ulcers.
5. Medication Administration
The "Five Rights":
Right patient, medication, dose, route, and time.
Techniques for administering oral, subcutaneous, intramuscular, and intravenous medications.
Use of infusion pumps and IV therapy safety.
6. Nutrition and Feeding
Assisting patients with meals, including those with swallowing difficulties.
Placement and care of nasogastric (NG) and percutaneous endoscopic gastrostomy (PEG) tubes.
Checking NG tube placement (pH testing, X-ray confirmation).
Prioritizing Patient Safety in Procedures
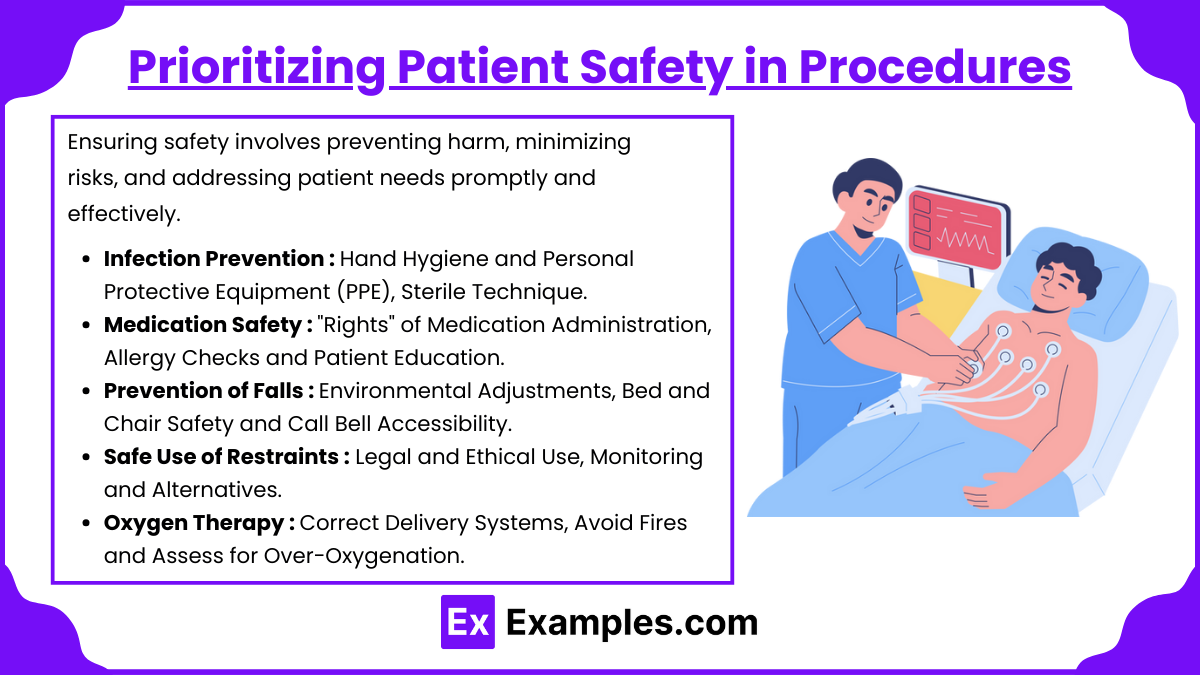
Patient safety is the cornerstone of nursing practice and is heavily emphasized in the NCLEX-RN® exam. Ensuring safety involves preventing harm, minimizing risks, and addressing patient needs promptly and effectively. Below are key considerations and strategies for prioritizing safety during nursing procedures:
1. Infection Prevention
Hand Hygiene: Perform handwashing or use alcohol-based hand rubs before and after patient contact, as well as during procedures, to reduce the risk of healthcare-associated infections (HAIs).
Personal Protective Equipment (PPE): Choose appropriate PPE (gloves, gowns, masks) based on the patient's condition and the type of procedure.
Sterile Technique: Follow sterile procedures during wound care, catheterization, and invasive interventions to prevent contamination.
2. Medication Safety
"Rights" of Medication Administration: Ensure the right patient, medication, dose, route, time, and documentation. Double-check high-alert medications (e.g., insulin, anticoagulants) with a second nurse.
Allergy Checks: Verify patient allergies before administering any medication, especially antibiotics or new drugs.
Patient Education: Inform patients about their medications, including potential side effects, to encourage adherence and report adverse reactions.
3. Prevention of Falls
Environmental Adjustments: Ensure a clutter-free environment, proper lighting, and secure assistive devices (walkers, canes).
Bed and Chair Safety: Keep the bed in the lowest position, brakes locked, and side rails up as necessary (without full restraint unless ordered).
Call Bell Accessibility: Place the call bell within the patient’s reach and respond promptly to minimize attempts to ambulate alone.
4. Safe Use of Restraints
Legal and Ethical Use: Use restraints only as a last resort and with a physician’s order. Ensure they are applied correctly to avoid injury.
Monitoring: Check for circulation, skin integrity, and signs of distress every 15–30 minutes. Release restraints every 2 hours to allow movement.
Alternatives: Encourage family presence, distraction techniques, and therapeutic interventions before applying restraints.
5. Oxygen Therapy
Correct Delivery Systems: Match oxygen delivery devices (nasal cannula, non-rebreather mask) to the patient’s needs while monitoring oxygen saturation.
Avoid Fires: Ensure no smoking or flammable substances are near oxygen equipment.
Assess for Over-Oxygenation: Monitor for oxygen toxicity, especially in long-term therapy patients.
Critical Tips for NCLEX Success
Excelling in the "Fundmentals: Skills/Procedures" section of the NCLEX-RN® exam requires a solid understanding of best practices and the ability to apply them efficiently. Below are critical tips to help you succeed in this domain:
Master Infection Control Protocols :
Follow Hand Hygiene Standards: Wash hands thoroughly before and after patient interactions or use alcohol-based hand sanitizer as appropriate.
Use PPE Correctly: Select and don the right personal protective equipment (gloves, gowns, masks) based on the patient's condition and the procedure being performed.
Practice Sterile Technique: Avoid breaks in sterility during invasive procedures, such as catheterization or wound care.
Always Prioritize Patient Safety:
Verify Patient Identity: Use two identifiers (e.g., name and date of birth) before administering medications or performing procedures.
Monitor for Adverse Reactions: Stay vigilant for potential complications, such as allergic reactions to medications or skin breakdown from devices.
Ensure Proper Positioning: Prevent pressure ulcers and respiratory complications by repositioning immobile patients every 2 hours.
Memorize Key Procedural Steps:
Vital Signs: Know how to accurately measure and interpret temperature, pulse, respiratory rate, and blood pressure.
Medication Administration: Memorize the "Rights of Medication Administration" and understand proper techniques for various routes (oral, subcutaneous, intramuscular, intravenous).
Wound Care: Understand dressing change protocols, wound assessment criteria, and the indications for advanced therapies like negative pressure wound therapy.
Use Prioritization Frameworks:
ABCs: Focus on Airway, Breathing, and Circulation when deciding the sequence of interventions.
Maslow’s Hierarchy of Needs: Address physiological needs before safety, love/belonging, or self-esteem concerns.
Time-Sensitive Procedures: Prioritize interventions with immediate impact on patient outcomes, such as administering insulin or oxygen therapy.
Practice Communication Skills :
Educate Patients: Clearly explain procedures, medications, and expected outcomes to enhance understanding and compliance.
Collaborate Effectively: Use the SBAR (Situation, Background, Assessment, Recommendation) method for concise and structured communication with the healthcare team.
Document Accurately: Record every intervention and observation to ensure continuity of care.
Examples
Example 1: Catheter Insertion and Care
The NCLEX-RN® often tests your ability to perform urinary catheterization, including the sterile technique required during insertion. You must recognize signs of infection, ensure proper catheter placement, and document the procedure accurately. Questions may involve troubleshooting complications like blockages or ensuring patient comfort while maintaining privacy.
Example 2: Vital Signs Monitoring
Assessing and interpreting vital signs such as temperature, pulse, respiratory rate, and blood pressure is a foundational skill. For example, you may encounter scenarios where abnormal values, like hypotension or tachycardia, require prioritization. The test may include questions about the appropriate response to specific vital sign abnormalities or monitoring trends over time.
Example 3: Wound Care Management
You may be asked about procedures for cleaning and dressing wounds, selecting appropriate dressings for specific wound types, and recognizing signs of infection or delayed healing. Understanding sterile versus clean techniques and using tools like wound VACs (vacuum-assisted closure) are frequently included in exam scenarios.
Example 4: Medication Administration
Safe administration of medications is a core nursing responsibility. The NCLEX-RN® evaluates your knowledge of the "rights" of medication administration, appropriate injection techniques, and the ability to identify adverse reactions. For instance, you might be required to calculate dosages or select the correct needle size and angle for an intramuscular injection.
Example 5: Patient Mobility and Transfer
Questions on proper body mechanics for transferring patients safely may appear, including the use of assistive devices like gait belts or mechanical lifts. The exam could also test your knowledge of interventions to prevent complications of immobility, such as pressure ulcers or deep vein thrombosis (DVT). Additionally, scenarios may focus on patient education for using mobility aids independently.
Practice Questions
Question 1
A nurse is preparing to administer a subcutaneous injection of insulin to a patient. Which of the following actions demonstrates proper technique?
A. Insert the needle at a 15° angle.
B. Use a 1½-inch needle for the injection.
C. Pinch the skin at the injection site before inserting the needle.
D. Aspirate before injecting the insulin.
Answer: C. Pinch the skin at the injection site before inserting the needle.
Explanation: Pinching the skin ensures that the medication is delivered into the subcutaneous tissue, not muscle. This technique is recommended for thin patients or areas with less subcutaneous fat.
Incorrect Options:
A. 15° angle: Subcutaneous injections should be administered at a 45° or 90° angle, depending on the patient's body size and fat distribution.
B. 1½-inch needle: A shorter needle (5/8 inch) is appropriate for subcutaneous injections.
D. Aspirating before injection: Aspiration is not necessary for subcutaneous insulin injections, as there is minimal risk of injecting into a blood vessel.
Question 2
A nurse is caring for a patient with an indwelling urinary catheter. What is the best nursing action to reduce the risk of infection?
A. Ensure the drainage bag is positioned above the bladder level.
B. Use sterile technique when emptying the drainage bag.
C. Secure the catheter tubing to the patient's leg.
D. Change the catheter daily to maintain sterility.
Answer: C. Secure the catheter tubing to the patient's leg.
Explanation: Securing the catheter tubing prevents tension on the catheter, reducing trauma to the urethra and the risk of infection.
Incorrect Options:
A. Drainage bag above the bladder: The drainage bag should always be below the bladder level to prevent backflow of urine, which can cause infection.
B. Use sterile technique: While sterile technique is important during insertion, clean technique is sufficient for emptying the drainage bag.
D. Change the catheter daily: Routine catheter changes are not recommended; they are performed only when clinically indicated.
Question 3
The nurse is teaching a patient how to use an incentive spirometer. Which of the following instructions should the nurse include?
A. "Exhale forcefully into the spirometer to improve lung expansion."
B. "Inhale slowly through the mouthpiece to raise the indicator."
C. "Use the spirometer only when you feel short of breath."
D. "Perform the exercise once daily for best results."
Answer: B. Inhale slowly through the mouthpiece to raise the indicator.
Explanation: Inhaling slowly through the spirometer helps expand the lungs and prevents atelectasis, especially after surgery or prolonged immobility. The patient should aim to raise the indicator to their goal level and hold their breath for 2–3 seconds to maximize lung expansion.
Incorrect Options:
A. Exhale forcefully: Incentive spirometry focuses on inhalation, not exhalation.
C. Use only when short of breath: The spirometer should be used regularly, not just when symptoms arise, to prevent complications.
D. Perform once daily: The patient should use the spirometer multiple times a day (e.g., 10 breaths per hour while awake).