Mastering Skills/Procedures is essential for success on the NCLEX-RN®, as these topics assess a nurse’s ability to effectively manage patient care, delegate tasks, and prioritize responsibilities. This section emphasizes critical thinking, clinical judgment, and applying theoretical knowledge in real-world scenarios. Key areas include delegation, prioritization, time management, leadership styles, and legal/ethical considerations. By focusing on these skills, nurses can ensure safe, efficient, and high-quality care while meeting the standards expected in professional practice. Proficiency in these concepts is vital for excelling on the NCLEX-RN®.
Learning Objectives
In studying "Leadership & Management: Skills/Procedures" for the NCLEX-RN®, you should learn to effectively delegate tasks, prioritize patient care, and manage time efficiently. Understand the principles behind the "5 Rights of Delegation," prioritization frameworks like ABC and Maslow’s Hierarchy, and strategies for conflict resolution. Evaluate leadership styles, including autocratic, democratic, and transformational approaches, and their application in different scenarios. Explore ethical and legal responsibilities such as advocacy, informed consent, and confidentiality. Apply your understanding to interpret complex patient care scenarios, ensuring safety, efficiency, and collaboration, as reflected in NCLEX-RN® practice passages and real-world nursing contexts.
Key Components of Leadership & Management in Nursing
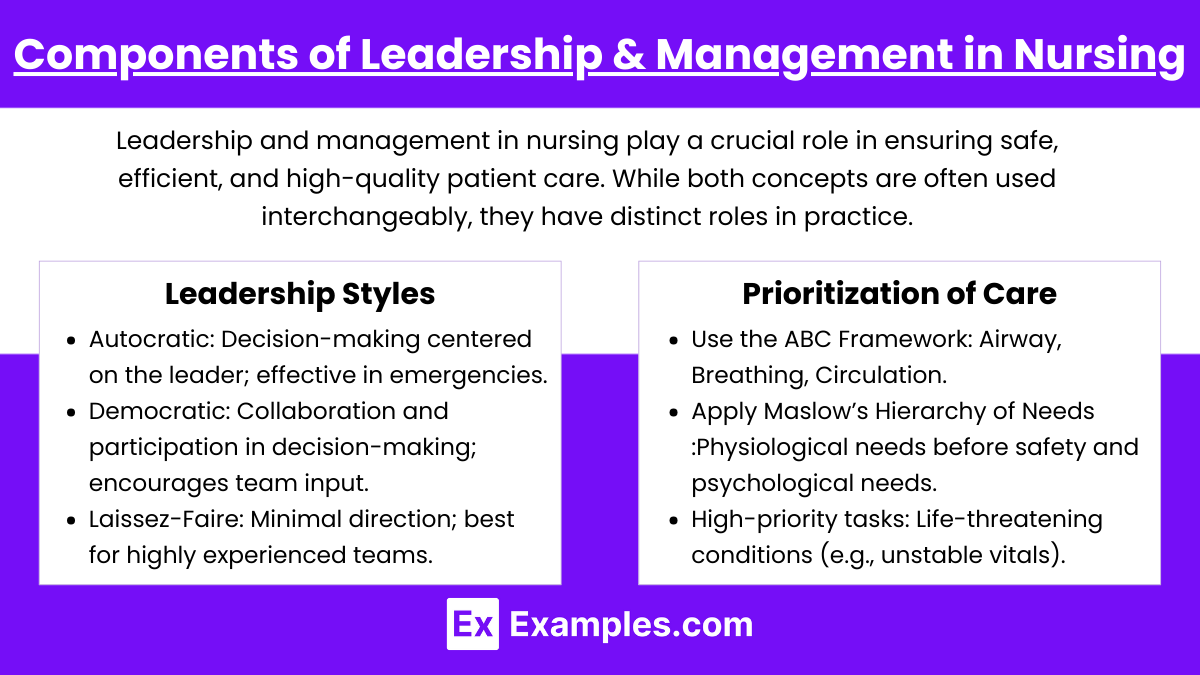
Leadership and management in nursing play a crucial role in ensuring safe, efficient, and high-quality patient care. While both concepts are often used interchangeably, they have distinct roles in practice. Nurse leaders inspire, motivate, and influence teams toward shared goals, while nurse managers handle operational aspects like staffing, budgeting, and policy implementation.
1. Leadership Styles
Autocratic: Decision-making centered on the leader; effective in emergencies.
Democratic: Collaboration and participation in decision-making; encourages team input.
Laissez-Faire: Minimal direction; best for highly experienced teams.
Transformational: Inspires and motivates staff to achieve goals.
Transactional: Focuses on task completion and rewards for performance.
2. Prioritization of Care
Use the ABC Framework: Airway, Breathing, Circulation.
Apply Maslow’s Hierarchy of Needs:
Physiological needs before safety and psychological needs.
Incorporate Urgency vs. Importance:
High-priority tasks: Life-threatening conditions (e.g., unstable vitals).
Low-priority tasks: Routine care that can be delegated.
Core Skills for Effective Management
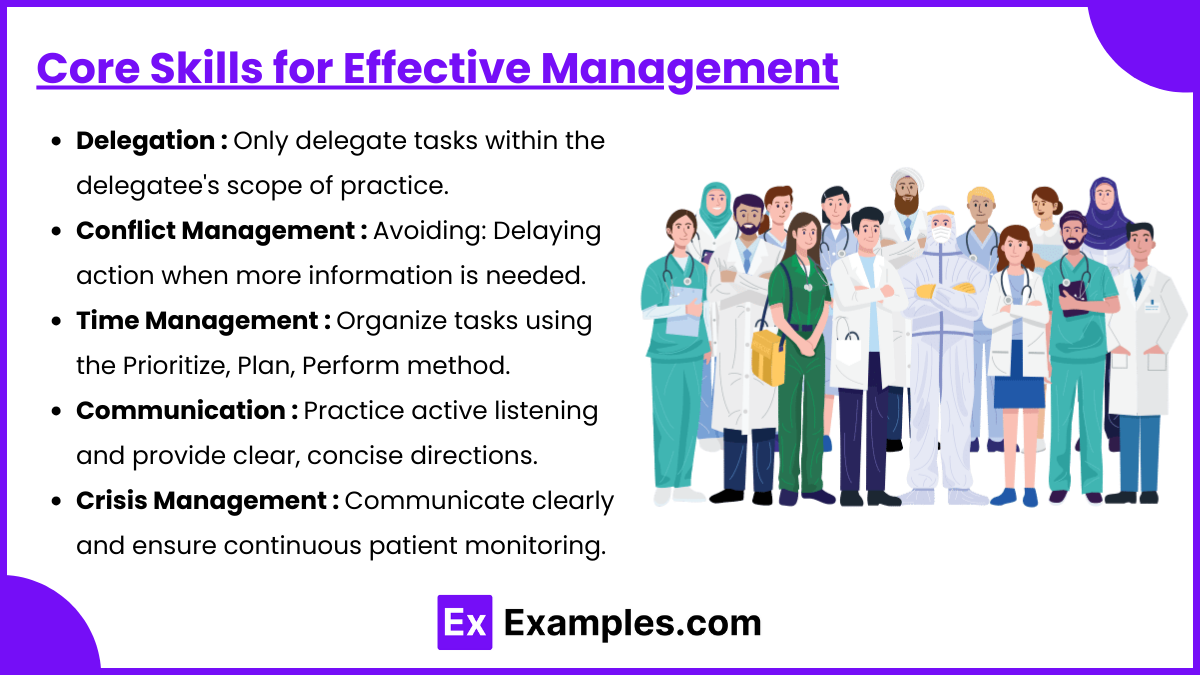
1. Delegation
Key Principles:
Only delegate tasks within the delegatee's scope of practice.
Ensure the right task, right circumstances, right person, right direction/communication, and right supervision/evaluation (5 Rights of Delegation).
Examples of Tasks to Delegate:
To Licensed Practical Nurses (LPNs): Dressing changes, medication administration (not IV push), Foley catheter insertion.
To Unlicensed Assistive Personnel (UAP): Vital signs, hygiene care, ambulation assistance.
2. Conflict Management
Approaches:
Avoiding: Delaying action when more information is needed.
Accommodating: Prioritizing team harmony over personal preferences.
Compromising: Finding a middle ground for conflicting parties.
Collaborating: Working together for a mutually beneficial solution.
3. Time Management
Organize tasks using the Prioritize, Plan, Perform method.
Cluster care to minimize interruptions.
Use delegation to focus on critical patient care.
4. Communication
Utilize SBAR Framework:
S: Situation – Describe the current issue.
B: Background – Provide context and patient history.
A: Assessment – State your findings.
R: Recommendation – Suggest next steps.
Practice active listening and provide clear, concise directions.
5. Crisis Management
Identify the crisis (e.g., Code Blue, mass casualty).
Mobilize resources and assign roles promptly.
Communicate clearly and ensure continuous patient monitoring.
Leadership & Management Procedures

1. Change Management : Change is inevitable in healthcare, and nurse leaders must guide their teams through transitions effectively. Lewin’s Change Theory is a widely used model for managing change in nursing practice. The three stages include
Lewin’s Change Theory:
Unfreeze: Recognize the need for change.
Change: Implement new strategies or protocols.
Refreeze: Solidify the new process as standard practice.
Engage staff through education and address resistance constructively.
2. Staff Education : Effective staff education ensures nurses maintain competency in new protocols, procedures, and evidence-based practices. Education improves patient care quality, enhances nurse confidence, and reduces errors. Key components of staff education include:
Conduct competency assessments.
Provide evidence-based training sessions.
Use feedback mechanisms to enhance learning.
3. Ethical and Legal Considerations : Nurse leaders and managers must uphold ethical and legal responsibilities in patient care. Ethical dilemmas often arise, requiring nurse managers to balance patient rights, safety, and organizational policies. Key considerations include:
Maintain patient confidentiality (HIPAA compliance).
Adhere to informed consent protocols.
Recognize ethical dilemmas and consult the ethics committee as needed.
4. Quality Improvement : Quality improvement (QI) is a structured process aimed at enhancing patient care, reducing errors, and optimizing healthcare outcomes. Nurse leaders and managers play a vital role in leading QI initiatives. Essential components of QI include:
Identify areas for improvement using data (e.g., fall rates, infection rates).
Implement Plan-Do-Study-Act (PDSA) cycles for continuous improvement.
Collaborate with the interdisciplinary team to review outcomes.
Examples
Example 1: Effective Delegation to Team Members
Delegation is a cornerstone of effective nursing leadership. For example, an RN may assign a Licensed Practical Nurse (LPN) to administer oral medications to stable patients or perform routine wound care while the RN focuses on critical patients requiring assessments or IV medication administration. Similarly, tasks such as measuring vital signs or assisting with hygiene can be delegated to Unlicensed Assistive Personnel (UAP), provided clear instructions are given and the RN maintains accountability. Understanding the 5 Rights of Delegation (right task, circumstance, person, communication, and supervision) ensures patient safety and adherence to legal and ethical standards.
Example 2: Prioritizing Care in Emergency Situations
In high-pressure scenarios, such as a mass casualty event or a patient experiencing cardiac arrest, prioritizing care becomes crucial. For instance, applying the ABC Framework (Airway, Breathing, Circulation) helps the nurse identify and address life-threatening issues first. An RN in charge of a unit during such an emergency would allocate resources efficiently, ensuring that critical patients receive immediate attention while delegating tasks for less urgent cases to appropriate team members. This demonstrates both clinical judgment and leadership in action.
Example 3: Conflict Resolution Among Team Members
Conflict resolution is a vital skill in managing healthcare teams. Suppose a disagreement arises between two nurses over the distribution of workload during a busy shift. As a leader, the RN can employ strategies such as active listening, mediation, and collaborative problem-solving to address the issue. For example, arranging a brief meeting to hear both sides and then proposing a fair and efficient plan demonstrates the RN’s ability to maintain harmony and team cohesion, which ultimately benefits patient care.
Example 4: Implementation of Quality Improvement Initiatives
Leadership often involves spearheading quality improvement initiatives. For example, an RN noticing an increase in hospital-acquired infections might lead a project to reduce infection rates. By organizing team meetings, educating staff on proper hand hygiene protocols, and monitoring compliance, the RN plays a leadership role in enhancing patient outcomes. The use of tools like the Plan-Do-Study-Act (PDSA) cycle exemplifies a structured approach to identifying problems, implementing changes, and evaluating outcomes.
Example 5: Crisis Management and Leadership During a Code Blue
In a Code Blue situation, effective leadership is essential to ensure timely and coordinated actions. For example, the RN leading the response would assign roles, such as chest compressions, defibrillation setup, and documentation, to team members. The leader maintains clear communication, often using structured frameworks like closed-loop communication, to confirm that instructions are heard and executed accurately. Post-event, the RN might conduct a debriefing session to review performance and identify areas for improvement, showcasing a commitment to both team development and patient safety.
Practice Questions
Question 1
A nurse is caring for multiple patients on a medical-surgical unit. Which task is appropriate to delegate to a UAP?
A. Administering insulin to a diabetic patient.
B. Assisting a stable patient with ambulation.
C. Educating a patient about wound care.
D. Performing a post-operative assessment.
Answer: B. Assisting a stable patient with ambulation.
Explanation:
Delegation Principles: The task must align with the UAP's scope of practice.
Right Task: Assisting a stable patient with ambulation is a routine, low-risk task suitable for delegation.
Incorrect Options:
A: Administering insulin is within the nurse's scope of practice and cannot be delegated to a UAP.
C: Patient education requires critical thinking and is the nurse's responsibility.
D: Post-operative assessments involve clinical judgment, which cannot be delegated.
Question 2
Which patient should the nurse assess first after receiving the shift report?
A. A patient with a blood pressure of 150/90 requesting pain medication for a headache.
B. A post-operative patient complaining of shortness of breath and chest pain.
C. A patient with a low-grade fever receiving IV antibiotics.
D. A patient with a history of diabetes requesting assistance to check blood sugar.
Answer: B. A post-operative patient complaining of shortness of breath and chest pain.
Explanation:
Prioritization Framework: Use the ABC (Airway, Breathing, Circulation) approach.
Rationale: Shortness of breath and chest pain are potential signs of a life-threatening condition such as a pulmonary embolism or myocardial infarction, requiring immediate intervention.
Incorrect Options:
A: Elevated blood pressure and headache are important but not immediately life-threatening.
C: A low-grade fever is concerning but not urgent in this context.
D: Checking blood sugar is important but does not take precedence over a potentially life-threatening condition.
Question 3
During a mass casualty incident in the emergency department, which leadership style is most appropriate for the charge nurse to use?
A. Laissez-faire
B. Democratic
C. Autocratic
D. Transformational
Answer: C. Autocratic
Explanation:
Leadership Style Suitability:
An autocratic leadership style is effective in emergencies requiring quick, decisive action without team input. The charge nurse must give clear instructions and maintain control to manage chaos effectively.
Incorrect Options:
A: Laissez-faire leadership lacks structure and is unsuitable in high-pressure situations.
B: Democratic leadership encourages team input, which is time-consuming and impractical in emergencies.
D: Transformational leadership inspires and motivates but may not be effective in urgent, fast-paced scenarios.