The urinary/renal system is a vital topic for the NCLEX RN® exam, as it encompasses critical functions like waste elimination, fluid and electrolyte balance, and blood pressure regulation. Understanding the anatomy, physiology, and common disorders of the renal system is essential for effective nursing care. Conditions such as acute kidney injury, chronic kidney disease, and urinary tract infections require knowledge of pathophysiology, diagnostic tools, and nursing interventions. Mastering this area enables nurses to provide comprehensive care and excel in NCLEX exam scenarios.
Learning Objectives
In studying “Urinary/Renal” for the NCLEX RN® exam, you should learn to understand the anatomy, physiology, and function of the urinary/renal system, including fluid and electrolyte regulation and waste excretion. Analyze the pathophysiology, clinical manifestations, and nursing interventions for common conditions like acute kidney injury, chronic kidney disease, and urinary tract infections. Evaluate principles of renal diagnostics, such as urinalysis and serum creatinine tests, and explore patient education strategies for preventing complications. Additionally, apply your understanding to prioritize nursing actions, interpret laboratory results, and manage care for patients with urinary or renal disorders in exam practice scenarios.
The urinary/renal system is a critical topic in the NCLEX RN® exam, especially within the adult health section. This area evaluates knowledge on renal function, common disorders, and nursing interventions to manage patients effectively. Below are detailed notes divided into three essential headings:
1. Anatomy and Physiology of the Urinary/Renal System
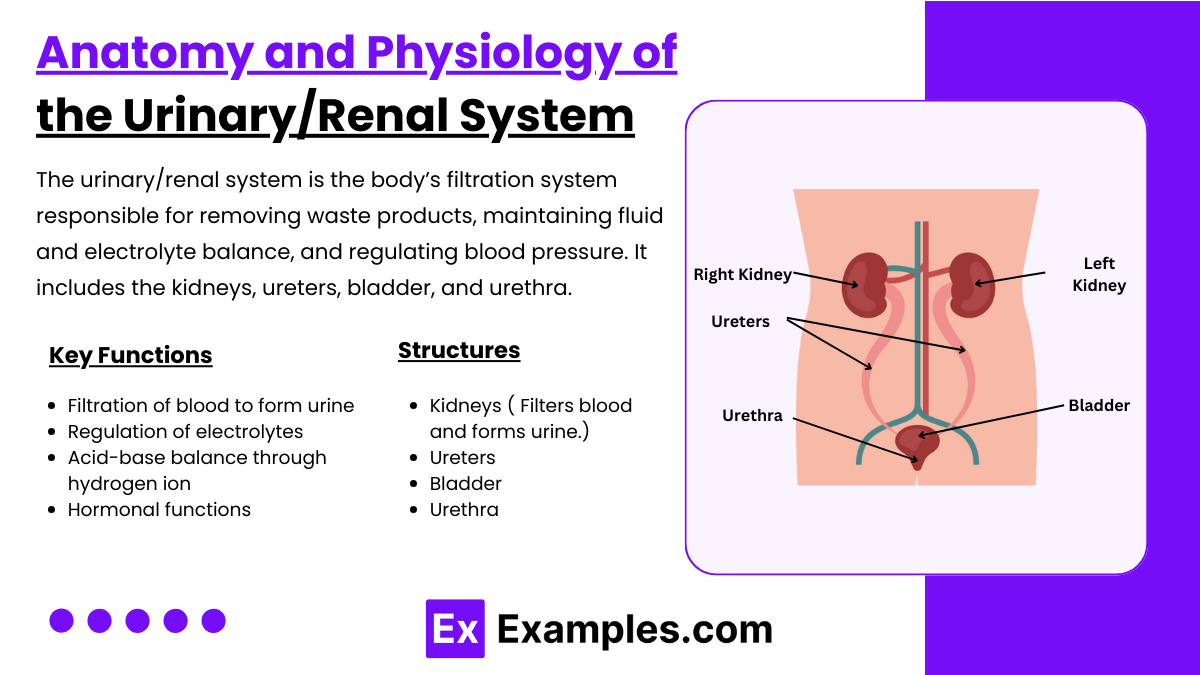
The urinary/renal system is the body’s filtration system responsible for removing waste products, maintaining fluid and electrolyte balance, and regulating blood pressure. It includes the kidneys, ureters, bladder, and urethra. The kidneys filter blood, forming urine, which is transported via ureters, stored in the bladder, and excreted through the urethra. Understanding the structure and function of the renal system is vital for effective nursing care.
- Kidney Functions:
- Filtration of blood to form urine (glomerular filtration rate or GFR).
- Regulation of electrolytes (e.g., sodium, potassium) and fluid balance.
- Acid-base balance through hydrogen ion and bicarbonate regulation.
- Hormonal functions (e.g., erythropoietin for RBC production, renin for blood pressure control, calcitriol for calcium metabolism).
- Structures:
- Kidneys: Filters blood and forms urine.
- Ureters: Transport urine from kidneys to the bladder.
- Bladder: Stores urine.
- Urethra: Excretes urine out of the body.
2. Common Disorders of the Urinary/Renal System
The urinary and renal systems play a vital role in maintaining fluid and electrolyte balance, filtering waste, and regulating blood pressure. For the NCLEX-RN® exam, it is crucial to understand common disorders, their pathophysiology, signs and symptoms, nursing interventions, and patient education. The NCLEX often focuses on the pathophysiology, signs and symptoms, diagnostics, and nursing care for these conditions.
a. Acute Kidney Injury (AKI):
- Definition: Sudden loss of kidney function due to ischemia, toxins, or sepsis.
- Phases:
- Initiation: Decreased GFR.
- Oliguric: Urine output <400 mL/day; elevated BUN/creatinine.
- Diuretic: Increased urine output with potential dehydration.
- Recovery: Gradual restoration of function.
- Nursing Interventions:
- Monitor fluid balance and daily weights.
- Administer diuretics or fluids as ordered.
- Restrict dietary sodium, potassium, and protein.
b. Chronic Kidney Disease (CKD):
- Definition: Progressive, irreversible loss of kidney function.
- Stages: Defined by GFR; End-Stage Renal Disease (ESRD) occurs when GFR <15 mL/min.
- Symptoms: Uremia, fluid overload, anemia, hyperkalemia, and metabolic acidosis.
- Management:
- Renal diet: Low protein, sodium, potassium, and phosphorus.
- Hemodialysis or peritoneal dialysis.
- Administer erythropoietin-stimulating agents for anemia.
c. Urinary Tract Infections (UTIs):
- Causes: E. coli is the most common pathogen.
- Symptoms:
- Dysuria, frequency, urgency, hematuria, suprapubic pain.
- In elderly: Confusion, incontinence.
- Treatment:
- Antibiotics (e.g., trimethoprim-sulfamethoxazole).
- Increase fluid intake.
- Educate on proper perineal hygiene.
3. Nursing Interventions and Patient Education
Nursing interventions and education strategies play a critical role in promoting recovery and preventing complications.
- Monitoring and Diagnostics:
- Labs: BUN, creatinine, GFR, urinalysis.
- Imaging: Renal ultrasound, CT scan, or cystoscopy.
- Daily Weights: Detect fluid retention.
- Preventive Care:
- Encourage hydration (2-3 L/day unless contraindicated).
- Teach proper toileting habits to prevent UTIs.
- Avoid nephrotoxic drugs (e.g., NSAIDs) in at-risk patients.
- Patient Education:
- Importance of adhering to prescribed dietary restrictions and medications.
- Monitoring for signs of worsening (e.g., decreased urine output, swelling, confusion).
- Techniques for managing urinary catheters or dialysis access sites.
- Acute Care Interventions:
- Strict intake and output monitoring.
- Administration of diuretics, antihypertensives, or electrolyte replacements as needed.
- Implement fall precautions for patients with uremia or confusion.
Examples
Example 1. Acute Kidney Injury (AKI)
Acute Kidney Injury is a sudden decline in renal function caused by factors such as hypovolemia, sepsis, or nephrotoxic medications. It is categorized into prerenal (reduced blood flow), intrarenal (damage to kidney tissues), and postrenal (obstruction of urine flow). NCLEX questions may focus on recognizing the oliguria phase, elevated BUN/creatinine levels, and hyperkalemia. Nursing interventions include fluid management, strict intake and output monitoring, and avoiding nephrotoxic drugs. The exam often tests prioritization, such as addressing life-threatening electrolyte imbalances or fluid overload.
Example 2. Chronic Kidney Disease (CKD)
Chronic Kidney Disease progresses over time, leading to irreversible renal failure if untreated. NCLEX scenarios may highlight stages of CKD, complications like uremia, or treatment modalities such as hemodialysis. Nursing care involves educating patients about dietary restrictions (low sodium, potassium, and phosphorus), monitoring for anemia, and assessing dialysis access sites for infection. Questions may also test the nurse’s ability to manage coexisting conditions like hypertension and diabetes, which exacerbate CKD progression.
Example 3. Urinary Tract Infections (UTIs)
UTIs are among the most common conditions tested in the urinary/renal system. They can range from uncomplicated cystitis to severe pyelonephritis. NCLEX questions often address risk factors such as urinary catheters, inadequate hygiene, or frequent sexual activity. Nurses must recognize symptoms like dysuria, frequency, and urgency, especially in vulnerable populations like the elderly, who may present with confusion instead. Interventions include administering antibiotics, encouraging increased fluid intake, and teaching preventive measures to reduce recurrence.
Example 4. Nephrotic Syndrome
Nephrotic syndrome is characterized by proteinuria, hypoalbuminemia, and severe edema due to glomerular damage. NCLEX questions may focus on its clinical presentation and complications, such as increased infection risk and thromboembolism. Nursing priorities include monitoring for edema, ensuring adequate nutritional intake (low sodium, moderate protein), and administering corticosteroids as prescribed. Patient education on preventing complications, such as reducing infection risk through hygiene and vaccination, is another critical focus.
Example 5. Urinary Incontinence
Urinary incontinence, particularly in older adults, is a significant topic in the NCLEX RN® exam. Types include stress incontinence (due to weak pelvic muscles) and urge incontinence (overactive bladder). Nurses must assess contributing factors like mobility issues or medications and provide appropriate interventions. These may include pelvic floor exercises (Kegels), bladder training programs, and dietary modifications to avoid irritants like caffeine. Questions may test the nurse’s ability to implement a care plan promoting dignity and independence while managing incontinence effectively.
Practice Questions
Question 1
A nurse is caring for a patient with acute kidney injury (AKI) in the oliguric phase. Which of the following findings would the nurse expect?
A. Polyuria
B. Hypokalemia
C. Increased BUN and creatinine levels
D. Metabolic alkalosis
Answer: C. Increased BUN and creatinine levels
Explanation:
- Oliguric phase of AKI: Urine output decreases to <400 mL/day, causing waste products to accumulate in the blood.
- Increased BUN and creatinine: These are hallmark indicators of impaired kidney function due to decreased filtration.
- Incorrect Options:
- A. Polyuria: This is seen in the diuretic phase of AKI, not the oliguric phase.
- B. Hypokalemia: The oliguric phase is associated with hyperkalemia due to reduced potassium excretion.
- D. Metabolic alkalosis: The oliguric phase often leads to metabolic acidosis because the kidneys cannot excrete hydrogen ions effectively.
Question 2
A nurse is providing discharge teaching to a patient with chronic kidney disease (CKD). Which dietary recommendation should the nurse include?
A. Increase potassium-rich foods like bananas and oranges.
B. Consume a low-protein diet unless on dialysis.
C. Restrict calcium intake to avoid hypercalcemia.
D. Increase fluid intake to at least 3 liters daily.
Answer: B. Consume a low-protein diet unless on dialysis.
Explanation:
- CKD and protein intake: Protein metabolism produces urea, which the kidneys cannot excrete effectively. A low-protein diet reduces this burden. However, patients on dialysis require increased protein to compensate for losses during treatment.
- Incorrect Options:
- A. Increase potassium-rich foods: CKD patients should avoid potassium-rich foods due to the risk of hyperkalemia.
- C. Restrict calcium intake: CKD patients are at risk for hypocalcemia due to impaired vitamin D activation, so calcium intake may need to be supported.
- D. Increase fluid intake: Fluid intake is often restricted in CKD to prevent fluid overload.
Question 3
A patient with a urinary tract infection (UTI) reports dysuria, urgency, and cloudy urine. Which intervention should the nurse prioritize?
A. Administer prescribed antibiotics.
B. Encourage a high-protein diet.
C. Instruct the patient to limit fluid intake.
D. Collect a blood culture before administering antibiotics.
Answer: A. Administer prescribed antibiotics.
Explanation:
- UTI management: The priority intervention is to administer antibiotics to treat the infection. Symptoms like dysuria, urgency, and cloudy urine indicate an active infection requiring prompt treatment.
- Incorrect Options:
- B. Encourage a high-protein diet: While protein is essential for healing, this is not a priority intervention for UTIs.
- C. Instruct the patient to limit fluid intake: Increased fluid intake is encouraged to flush out bacteria from the urinary tract.
- D. Collect a blood culture before administering antibiotics: Blood cultures are unnecessary for uncomplicated UTIs. Urine culture may be needed before starting antibiotics in some cases.