The urinary/renal system plays a vital role in maintaining homeostasis by regulating fluid and electrolyte balance, removing waste products, and controlling blood pressure. In critical care settings, conditions such as acute kidney injury (AKI), chronic kidney disease (CKD), and electrolyte imbalances require immediate assessment and intervention. Nurses must monitor for complications, interpret diagnostic findings, and provide timely treatments like dialysis. Mastery of urinary/renal concepts is essential for the NCLEX-RN®, as it ensures the ability to prioritize care and promote optimal patient outcomes in high-stakes scenarios.
Learning Objectives
In studying “Critical Care: Urinary/Renal” for the NCLEX-RN® exam, you should learn to assess and manage renal dysfunction, including acute kidney injury (AKI), chronic kidney disease (CKD), and electrolyte imbalances. Understand diagnostic tests such as urinalysis, BUN, and creatinine levels to evaluate renal function. Explore interventions like fluid management, dialysis modalities, and pharmacological treatments for hyperkalemia, acidosis, and fluid overload. Analyze the principles of hemodynamic monitoring, catheter care, and infection prevention. Additionally, apply your understanding to clinical scenarios involving renal emergencies, fluid and electrolyte disturbances, and interpret data to prioritize safe, evidence-based care in critical care nursing practice.
Common Urinary/Renal Conditions in Critical Care
Managing urinary and renal conditions in critical care is essential for patient outcomes, particularly as these conditions can rapidly worsen without prompt intervention. Below are the key conditions encountered in critical care:
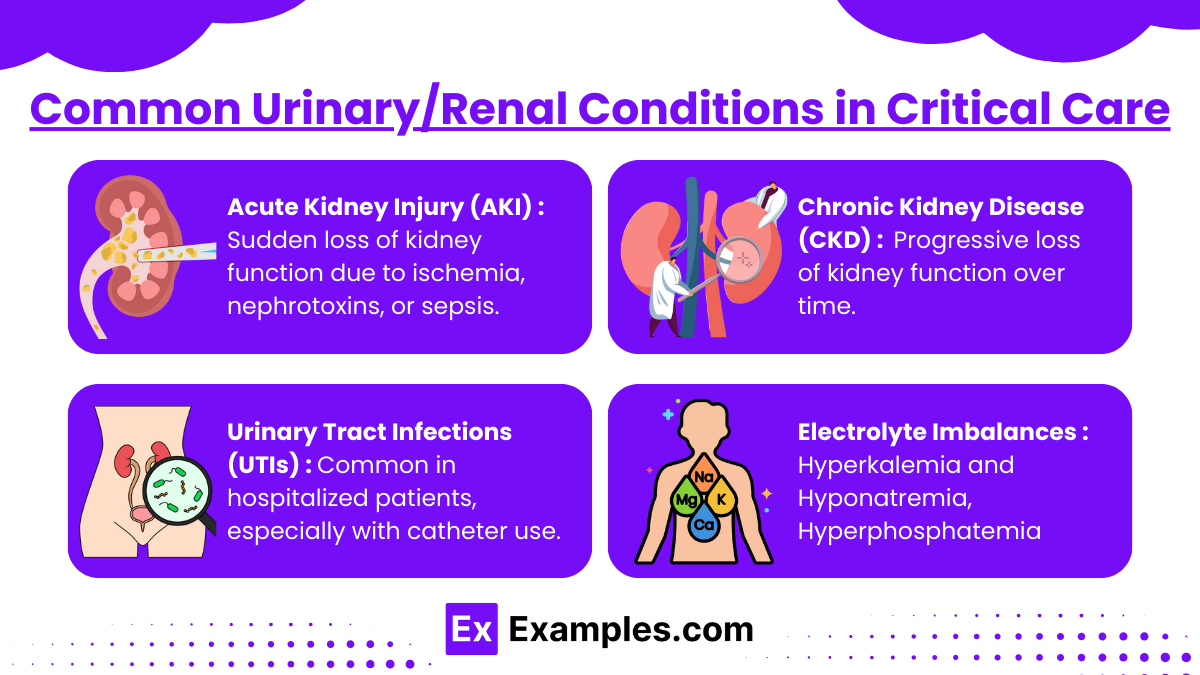
1. Acute Kidney Injury (AKI):
- Sudden loss of kidney function due to ischemia, nephrotoxins, or sepsis.
- Types: Pre-renal (decreased perfusion), Intra-renal (damage to kidney tissue), and Post-renal (obstruction).
- Key signs: Elevated BUN and creatinine, decreased urine output, and electrolyte imbalances (hyperkalemia, hyponatremia).
2. Chronic Kidney Disease (CKD):
- Progressive loss of kidney function over time.
- Signs: Fatigue, anemia, fluid overload, and metabolic acidosis.
3. Urinary Tract Infections (UTIs):
- Common in hospitalized patients, especially with catheter use.
- Symptoms: Dysuria, urgency, fever, and suprapubic pain.
- Preventable by using sterile techniques for catheter insertion and maintenance.
4. Electrolyte Imbalances:
- Hyperkalemia: ECG changes (peaked T waves), muscle weakness.
- Hyponatremia: Confusion, seizures, edema.
- Hyperphosphatemia: Related to CKD, leading to calcium deposits and bone disorders.
Nursing Care and Interventions
- Assessment and Monitoring : Monitoring and assessing urinary and renal function is critical in managing patients in a critical care setting. Nurses should carefully observe urine output, ensuring it meets the minimum standard of 30 mL/hr, which indicates adequate kidney perfusion. Regular evaluation of lab values, including BUN, creatinine, GFR, and electrolytes, provides insights into kidney function and potential imbalances. Assessing fluid status is equally important—watch for signs of fluid overload, such as edema, crackles in the lungs, or jugular vein distension, and for symptoms of dehydration, including dry mucous membranes, hypotension, and concentrated urine. Vital signs should also be monitored consistently, as hypertension is common in CKD, while hypotension may indicate pre-renal AKI.
- Management of Acute Kidney Injury (AKI) : Effective management of AKI and CKD involves targeted interventions based on the underlying condition. For pre-renal AKI, ensuring proper hydration with cautious administration of IV fluids can improve kidney perfusion. In cases of CKD or AKI, avoiding nephrotoxic drugs, such as NSAIDs and aminoglycosides, is crucial to prevent further kidney damage. Fluid overload may require the use of loop diuretics like furosemide to reduce pulmonary edema and systemic retention. Electrolyte imbalances need prompt correction, particularly hyperkalemia, which can be managed with Kayexalate, insulin with glucose, or calcium gluconate. Hyperphosphatemia can be addressed using phosphate binders like sevelamer, while hyponatremia may necessitate cautious use of hypertonic saline in severe cases.
- Preventing Infections : Preventing infections, particularly urinary tract infections (UTIs), is a vital aspect of nursing care. Strict adherence to aseptic technique during catheter insertion and care is necessary to minimize infection risks. Indwelling catheters should be removed as soon as they are no longer needed to reduce prolonged exposure to pathogens. Proper hygiene practices, such as regular perineal care, should be encouraged for incontinent patients, and those prone to recurrent UTIs should be educated on maintaining good hygiene. Nurses must remain vigilant for signs of infection, such as fever, dysuria, foul-smelling urine, or cloudy urine, and act promptly to manage potential complications.
- Dietary Management : Dietary adjustments are an integral part of managing renal conditions. A low-potassium diet is essential to avoid complications like hyperkalemia, which can cause life-threatening arrhythmias. Foods high in potassium, such as bananas, oranges, and spinach, should be restricted. For patients with CKD, protein intake may need to be moderated to reduce the strain on the kidneys, while sodium restriction can help manage fluid retention and hypertension. Collaboration with a dietitian can ensure that patients receive a tailored diet plan that aligns with their specific renal condition and treatment goals.
Strategies for Urinary/Renal Questions
The urinary/renal system questions on the NCLEX RN® often assess your ability to prioritize care, recognize critical conditions, and implement appropriate interventions. Below are practical strategies to help you answer these questions effectively:
1. Prioritize Based on the ABCs (Airway, Breathing, Circulation)
- Always focus on life-threatening issues first, such as:
- Fluid overload leading to pulmonary edema (monitor breathing).
- Hyperkalemia causing arrhythmias (monitor circulation).
- Example: A question about hyperkalemia symptoms requires recognizing peaked T waves on an ECG and acting to prevent cardiac arrest.
2. Apply the Nursing Process:
Use the ADPIE framework (Assessment, Diagnosis, Planning, Implementation, Evaluation) to break down the question logically:
- Assessment First: Look for key clues in patient data (e.g., urine output <30 mL/hr, elevated creatinine).
- Implementation: Prioritize interventions aligned with the condition, such as administering diuretics or adjusting IV fluids.
3. Watch for Lab Value Trends:
- Understand normal ranges for renal function indicators:
- BUN: 7–20 mg/dL
- Creatinine: 0.6–1.2 mg/dL
- GFR: >90 mL/min
- Potassium: 3.5–5.0 mEq/L
- Questions often include abnormal labs to direct your attention to the root cause of the problem.
4. Recognize Signs of Complications:
- Acute Kidney Injury (AKI):
- Look for decreased urine output, fluid retention, or electrolyte imbalances.
- Chronic Kidney Disease (CKD):
- Prioritize interventions for anemia, hyperphosphatemia, and fluid overload.
- UTIs: Identify fever, dysuria, or confusion in elderly patients as warning signs of sepsis.
5. Prioritize Safety and Prevention:
- Focus on interventions that prevent harm:
- For patients with indwelling catheters, prioritize sterile technique and removal when no longer needed.
- For CKD patients, teach low-protein and low-potassium diets to prevent complications.
Examples
Example 1. Managing Acute Kidney Injury (AKI)
A patient in the oliguric phase of AKI presents with reduced urine output, elevated serum potassium, and metabolic acidosis. The nurse must prioritize interventions to prevent complications such as hyperkalemia-induced arrhythmias. This includes administering IV calcium gluconate, insulin with glucose, and preparing the patient for possible dialysis while monitoring strict intake and output (I&O).
Example 2. Responding to Fluid Overload in Chronic Kidney Disease (CKD)
A patient with CKD exhibits signs of fluid overload, including pulmonary crackles, dyspnea, and peripheral edema. The nurse must implement fluid restrictions, administer prescribed diuretics, and elevate the head of the bed to promote oxygenation. Continuous monitoring of daily weight and serum electrolytes is critical to evaluate treatment effectiveness and prevent worsening of symptoms.
Example 3. Hyperkalemia Management in a Hemodialysis Patient
A patient undergoing hemodialysis reports muscle weakness and is found to have a potassium level of 6.8 mEq/L. The nurse should immediately administer emergency interventions, such as IV insulin with dextrose and sodium polystyrene sulfonate (Kayexalate), while preparing for dialysis. Close monitoring of cardiac rhythms is essential to prevent life-threatening arrhythmias.
Example 4. Urinary Tract Infection (UTI) Leading to Urosepsis
A catheterized patient in critical care develops fever, hypotension, and altered mental status, indicative of urosepsis. The nurse must obtain a urine culture, initiate broad-spectrum antibiotics as prescribed, and monitor vital signs closely. Preventive measures, such as meticulous catheter care and encouraging adequate fluid intake, are essential to reduce recurrence.
Example 5. Peritonitis in Peritoneal Dialysis
A patient receiving peritoneal dialysis reports cloudy effluent and severe abdominal pain, signs of peritonitis. The nurse must notify the healthcare provider, prepare to administer intraperitoneal antibiotics, and educate the patient on aseptic techniques for dialysis exchanges. This scenario emphasizes the importance of recognizing early signs of complications and acting promptly to prevent further deterioration.
Practice Questions
Question 1
A nurse is caring for a patient with acute kidney injury (AKI) who is in the oliguric phase. Which intervention should the nurse prioritize?
A. Encourage the patient to drink at least 2 liters of fluid daily.
B. Administer a diuretic to increase urine output as prescribed.
C. Restrict potassium-rich foods and monitor cardiac rhythm.
D. Prepare the patient for hemodialysis immediately.
Answer: C. Restrict potassium-rich foods and monitor cardiac rhythm.
Explanation:
- During the oliguric phase of AKI, the kidneys are unable to excrete potassium effectively, leading to hyperkalemia, which can cause life-threatening cardiac arrhythmias.
- Potassium restriction and cardiac monitoring are essential nursing interventions to prevent complications.
- Option A is inappropriate because fluid intake should be restricted during the oliguric phase to prevent fluid overload.
- Option B may be prescribed but is not the first priority compared to addressing hyperkalemia.
- Option D is a possibility if hyperkalemia becomes severe, but dialysis is not always immediately necessary.
Question 2
A patient undergoing hemodialysis reports feeling lightheaded and dizzy during the procedure. What is the most appropriate initial nursing action?
A. Stop the dialysis and notify the healthcare provider.
B. Administer a bolus of IV saline as prescribed.
C. Place the patient in Trendelenburg position.
D. Assess the patient’s blood pressure and reduce the rate of fluid removal.
Answer: D. Assess the patient’s blood pressure and reduce the rate of fluid removal.
Explanation:
- Lightheadedness and dizziness during hemodialysis are often caused by hypotension due to rapid fluid removal.
- The nurse should first assess the patient’s blood pressure to confirm hypotension and then reduce the rate of fluid removal to stabilize the patient.
- Option A is incorrect because stopping the dialysis may not be necessary and should only be done if hypotension persists.
- Option B may be appropriate later if hypotension is confirmed and prescribed.
- Option C (Trendelenburg position) is not routinely recommended for managing dialysis-related hypotension.
Question 3
A patient with chronic kidney disease (CKD) is being educated about dietary restrictions. Which statement by the patient indicates a need for further teaching?
A. “I will avoid bananas and oranges to limit my potassium intake.”
B. “I will reduce my salt intake to help control my blood pressure.”
C. “I should increase my protein intake to help with energy.”
D. “I will limit my fluid intake to avoid swelling and weight gain.”
Answer: C. “I should increase my protein intake to help with energy.”
Explanation:
- In CKD, excessive protein intake should be avoided because it increases the production of urea, a waste product that the kidneys cannot effectively excrete.
- Option A demonstrates correct understanding of potassium restriction to prevent hyperkalemia.
- Option B is correct as reducing salt helps control hypertension, a common complication of CKD.
- Option D is correct because fluid restriction helps prevent fluid overload and associated complications like pulmonary edema.