The visual and auditory systems play essential roles in sensory perception, enabling individuals to interact with their environment. The NCLEX-RN® exam emphasizes understanding these systems’ anatomy, physiology, and common disorders, such as glaucoma, cataracts, hearing loss, and Meniere’s disease. Nurses must assess and manage conditions using diagnostic tools, therapeutic interventions, and patient education to promote safety and quality of life. Mastery of these concepts ensures effective care for patients with sensory impairments and enhances critical thinking in clinical scenarios, a vital skill for NCLEX success.
In studying “Visual/Auditory” for the NCLEX-RN® exam, you should learn to assess and manage conditions affecting the visual and auditory systems, such as glaucoma, cataracts, macular degeneration, and hearing loss. Understand the anatomy and physiology of these systems, the pathophysiology of common disorders, and nursing interventions, including medication administration, patient education, and safety measures. Evaluate diagnostic tools like Snellen charts, Rinne and Weber tests, and otoscopic exams. Additionally, explore strategies to support patients with sensory impairments and apply your understanding to prioritize care, prevent complications, and interpret clinical scenarios in NCLEX-style practice questions.
Visual System
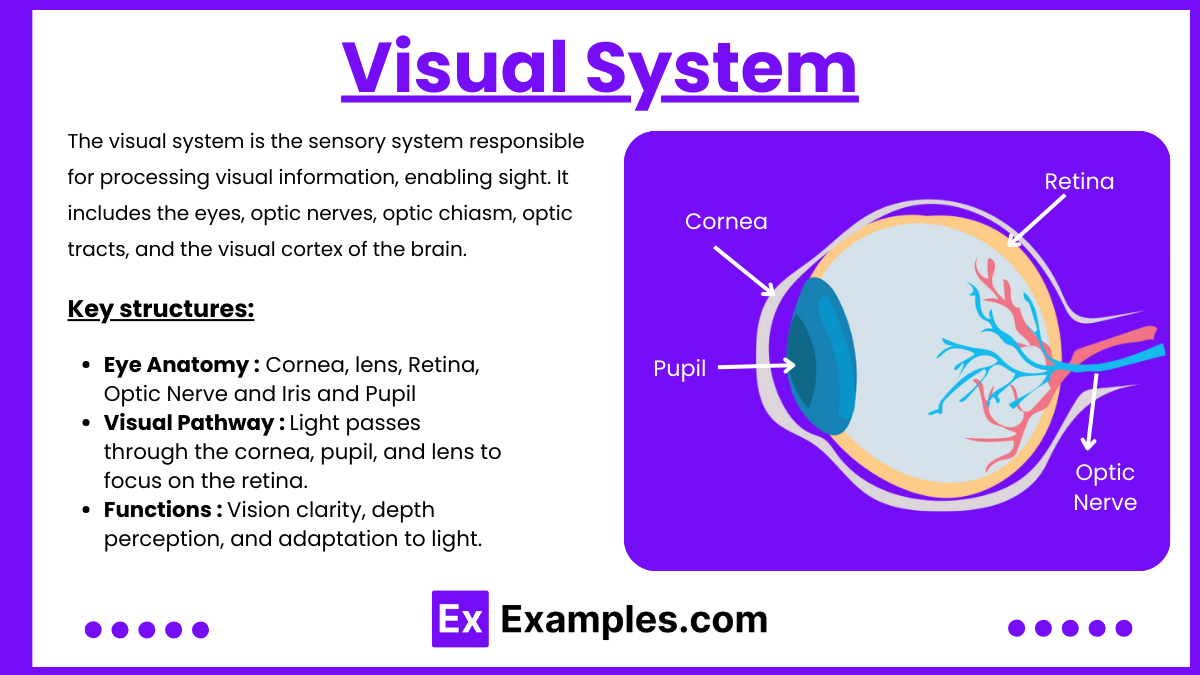
The visual system is the sensory system responsible for processing visual information, enabling sight. It includes the eyes, optic nerves, optic chiasm, optic tracts, and the visual cortex of the brain. The eyes capture light, convert it into electrical signals, and transmit these signals to the brain for interpretation, allowing perception of images, color, and depth.
Key structures:
- Eye Anatomy:
- Cornea: Transparent layer that focuses light.
- Lens: Adjusts focus for near and far objects.
- Retina: Contains photoreceptors (rods for dim light and cones for color vision).
- Optic Nerve: Transmits signals from the retina to the brain.
- Iris and Pupil: Regulate light entry.
- Visual Pathway:
- Light passes through the cornea, pupil, and lens to focus on the retina.
- The retina’s photoreceptors convert light into neural signals, sent to the brain via the optic nerve.
- Functions:
- Vision clarity, depth perception, and adaptation to light.
Auditory System
The auditory system refers to the complex network of anatomical structures and physiological processes responsible for hearing. It includes the outer ear (collects sound waves), middle ear (amplifies vibrations), inner ear (converts vibrations to neural signals), and the auditory nerve that transmits these signals to the brain for interpretation. The system enables sound detection, localization, and processing, playing a critical role in communication and environmental awareness. The auditory system processes sound waves and maintains balance.
key components
- Outer Ear:
- Pinna (Auricle): Collects sound waves.
- External Auditory Canal: Directs sound to the eardrum.
- Middle Ear:
- Tympanic Membrane (Eardrum): Vibrates in response to sound.
- Ossicles: Amplify sound vibrations (malleus, incus, stapes).
- Inner Ear:
- Cochlea: Converts vibrations into neural signals for hearing.
- Semicircular Canals: Regulate balance and spatial orientation.
- Auditory Pathway:
- Sound waves are converted into electrical signals transmitted to the brain via the auditory nerve.
Common Disorders of the Visual System
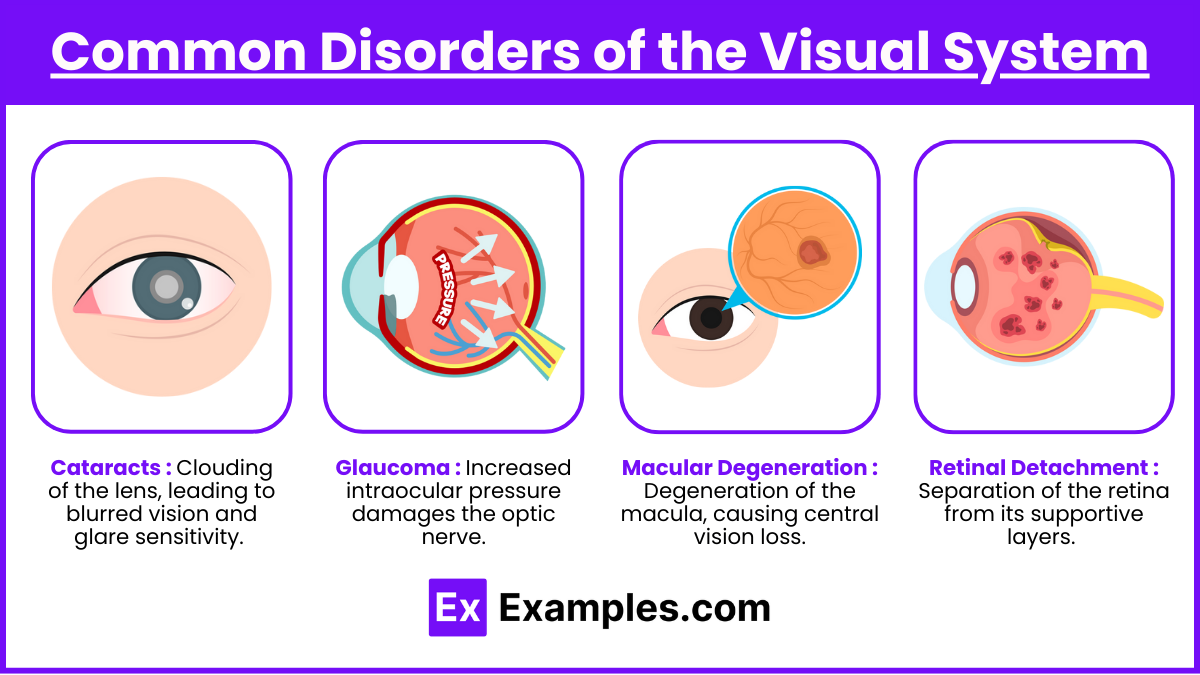
- Cataracts:
- Clouding of the lens, leading to blurred vision and glare sensitivity.
- Common causes: Aging, UV exposure, diabetes.
- Glaucoma:
- Increased intraocular pressure damages the optic nerve.
- Open-angle: Gradual peripheral vision loss.
- Angle-closure: Sudden onset, medical emergency.
- Macular Degeneration:
- Degeneration of the macula, causing central vision loss.
- Dry Type: Slow, progressive loss.
- Wet Type: Rapid loss with abnormal blood vessel growth.
- Retinal Detachment:
- Separation of the retina from its supportive layers.
- Symptoms include flashes of light, floaters, or shadowed vision.
Common Disorders of the Auditory System
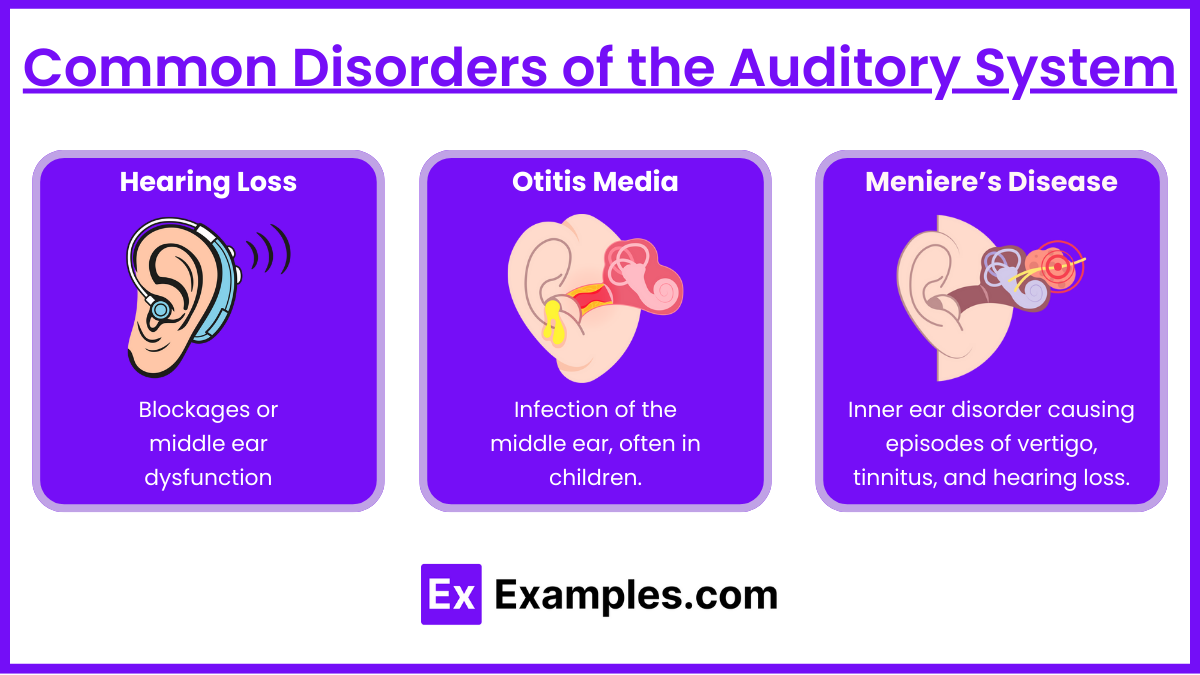
- Hearing Loss:
- Conductive: Blockages or middle ear dysfunction (e.g., cerumen impaction).
- Sensorineural: Damage to inner ear or auditory nerve (e.g., presbycusis).
- Otitis Media:
- Infection of the middle ear, often in children.
- Symptoms: Pain, fever, hearing impairment.
- Meniere’s Disease:
- Inner ear disorder causing episodes of vertigo, tinnitus, and hearing loss.
- Triggered by fluid imbalance in the inner ear.
Nursing Interventions for Visual and Auditory Disorders

Nursing interventions for visual and auditory disorders focus on promoting safety, improving communication, enhancing quality of life, and preventing complications. Below is a comprehensive guide to interventions that address both sensory systems:
1. Promote Patient Safety
- Create a safe environment to reduce the risk of injuries due to impaired vision or hearing:
- Visual Disorders: Remove tripping hazards, use contrasting colors for better visibility, and ensure adequate lighting.
- Auditory Disorders: Minimize background noise and use flashing lights for alarms or doorbells.
- Encourage the use of assistive devices:
- Glasses, magnifiers, or contact lenses for visual impairments.
- Hearing aids or cochlear implants for hearing loss.
2. Enhance Communication
- Use strategies to facilitate effective interaction:
- For visual impairments: Provide verbal explanations and tactile cues when communicating or teaching.
- For hearing impairments: Face the patient while speaking, use written instructions or visual aids, and encourage lip-reading or sign language if applicable.
- Ensure clear, concise communication:
- Speak clearly and at an appropriate volume, avoiding shouting, which may distort sound for hearing-impaired patients.
3. Patient Education
- Teach proper use and maintenance of medical devices:
- Visual: Demonstrate eye drop application for conditions like glaucoma and post-cataract surgery care.
- Auditory: Educate on the care and cleaning of hearing aids.
- Emphasize the importance of routine screenings:
- Regular eye exams for early detection of visual conditions.
- Hearing tests to monitor or prevent hearing loss progression.
- Provide condition-specific education:
- Visual Disorders: Explain signs of complications like increased intraocular pressure (glaucoma) or infection (post-surgery).
- Auditory Disorders: Discuss triggers for vertigo (e.g., high salt intake in Meniere’s disease) and the importance of early treatment for infections like otitis media.
4. Prevent Complications
- Administer medications as prescribed:
- Visual Disorders: Timolol for glaucoma, antibiotics post-eye surgery.
- Auditory Disorders: Antibiotics for otitis media, antiemetics or diuretics for Meniere’s disease.
- Monitor for adverse effects of treatments and provide timely interventions.
- Position the patient appropriately for certain conditions:
- Visual: Maintain head positioning for retinal detachment post-surgery.
- Auditory: Assist patients with vertigo to avoid sudden movements.
5. Promote Independence
- Encourage the use of assistive technologies:
- Magnification tools, talking devices, or mobility aids for visually impaired patients.
- Amplified telephones and alerting systems for hearing-impaired patients.
- Collaborate with occupational therapists to provide training in using these aids effectively
Examples
Example 1. A Patient with Glaucoma
A 65-year-old patient is diagnosed with open-angle glaucoma and is prescribed timolol eye drops to lower intraocular pressure (IOP). The nurse educates the patient about the importance of lifelong treatment to prevent optic nerve damage and progressive vision loss. The patient is taught proper eye drop administration techniques, including hand hygiene, avoiding touching the dropper tip to the eye, and waiting at least five minutes before administering additional eye medications. The nurse also emphasizes the importance of routine follow-up visits to monitor IOP and prevent complications.
Example 2. A Patient with Retinal Detachment
A 55-year-old patient presents with complaints of sudden flashes of light, floaters, and a “curtain-like” shadow over their vision in one eye. The nurse recognizes these as symptoms of retinal detachment, a medical emergency, and promptly notifies the healthcare provider. The nurse prepares the patient for possible surgical intervention, explains the need for head positioning based on the detachment location, and advises the patient to avoid activities that could worsen the condition, such as heavy lifting or straining.
Example 3. A Patient with Cataract Surgery
A 72-year-old patient undergoes cataract removal and intraocular lens implantation. Postoperatively, the nurse provides discharge teaching, including instructions to wear an eye shield at night, avoid rubbing the eye, and refrain from activities that increase intraocular pressure, such as bending or heavy lifting. The nurse also reviews the proper use of prescribed antibiotic and anti-inflammatory eye drops. The patient is advised to report symptoms such as severe pain, increased redness, or vision changes, which may indicate complications like infection or increased intraocular pressure.
Example 4. A Patient with Meniere’s Disease
A 50-year-old patient reports recurrent episodes of vertigo, tinnitus, and hearing loss, consistent with Meniere’s disease. The nurse educates the patient about dietary modifications, including a low-sodium diet to reduce fluid retention in the inner ear. The nurse also discusses the use of prescribed medications such as meclizine for vertigo and diuretics to manage symptoms. Additionally, the patient is taught fall prevention strategies, such as sitting or lying down during vertigo episodes and avoiding sudden head movements.
Example 5. A Patient with Otitis Media
A 40-year-old patient presents with ear pain, fever, and muffled hearing, diagnosed as acute otitis media. The nurse administers prescribed antibiotics and analgesics to manage infection and pain. Patient teaching includes completing the full course of antibiotics to prevent complications such as hearing loss or the spread of infection. The nurse also educates the patient on measures to prevent recurrence, such as avoiding exposure to secondhand smoke and treating upper respiratory infections promptly.
Practice Questions
Question 1
A patient with open-angle glaucoma is prescribed timolol eye drops. What is the nurse’s priority teaching for this patient?
A. “Apply pressure to the inner corner of the eye after administering the drops.”
B. “Keep the bottle refrigerated to preserve the medication.”
C. “Administer the drops as needed when your eyes feel irritated.”
D. “Avoid blinking after applying the drops to prevent loss of medication.
Answer: A. “Apply pressure to the inner corner of the eye after administering the drops.”
Explanation: Applying pressure to the nasolacrimal duct (inner corner of the eye) for 1-2 minutes prevents systemic absorption of timolol, reducing side effects like bradycardia and hypotension.
Why others are incorrect:
- B: Most eye drops do not require refrigeration unless specifically instructed.
- C: Glaucoma medications must be administered regularly, not as needed.
- D: While excessive blinking may dislodge drops, it is not the primary concern compared to systemic absorption.
Question 2
A patient is experiencing sudden flashes of light and a curtain-like shadow over their visual field. What should the nurse do first?
A. Encourage the patient to rest with their eyes closed.
B. Place the patient in a dark room to reduce visual stimulation.
C. Position the patient so the head is immobilized and alert the provider immediately.
D. Administer prescribed eye drops to reduce intraocular pressure.
Answer: C. Position the patient so the head is immobilized and alert the provider immediately.
Explanation: These symptoms indicate a possible retinal detachment, a medical emergency requiring immediate surgical intervention. Immobilizing the head minimizes further damage.
Why others are incorrect:
- A: Resting with eyes closed does not address the urgency of retinal detachment.
- B: A dark room does not prevent further detachment or provide immediate care.
- D: Eye drops for intraocular pressure are not relevant unless the condition is glaucoma. Retinal detachment requires surgery.
Question 3
A patient with Meniere’s disease complains of severe vertigo and nausea. Which intervention should the nurse implement first?
A. Administer prescribed antiemetics and antivertigo medications.
B. Encourage the patient to walk slowly with assistance.
C. Restrict fluids to reduce inner ear pressure.
D. Instruct the patient to lie still and avoid sudden head movements.
Answer: D. Instruct the patient to lie still and avoid sudden head movements.
Explanation: The immediate priority is to reduce vertigo symptoms and prevent falls by instructing the patient to lie still and avoid movements that may worsen the symptoms.
Why others are incorrect:
- A: Administering medications is important but should follow non-pharmacological measures to stabilize the patient.
- B: Walking during a vertigo episode increases fall risk and should be avoided.
- C: Fluid restriction is not a first-line intervention during an acute episode; it is part of long-term management for Meniere’s disease.