Child health related to visual and auditory systems is a critical area for the NCLEX RN® exam, requiring nurses to identify, assess, and manage conditions that impact a child’s sensory development. Early detection and intervention are vital in preventing long-term complications such as developmental delays, social challenges, or impaired learning. Understanding common visual and auditory disorders, their risk factors, symptoms, and treatments ensures effective care delivery. Focus on nursing priorities, patient education, and appropriate interventions to promote optimal sensory health and developmental outcomes in children.
Learning Objectives
In studying “Child Health: Visual/Auditory” for the NCLEX RN® exam, you should learn to understand the common visual and auditory disorders in children, including refractive errors, strabismus, otitis media, and congenital hearing loss. Analyze the diagnostic techniques and treatment options for these conditions, such as patching, hearing aids, and surgical interventions. Evaluate the principles of developmental milestones and early screening methods to detect impairments. Additionally, explore how nursing interventions support early detection, parental education, and adherence to treatment plans. Apply your understanding to prioritize care, recognize complications, and interpret clinical scenarios in NCLEX RN® practice questions.
Visual and auditory health in children are critical areas in pediatric nursing. Early detection, assessment, and management of visual and auditory impairments can prevent long-term complications. For the NCLEX RN® exam, understanding common conditions, their nursing implications, and the relevant interventions will enhance your ability to prioritize care and answer related questions effectively.
Visual Disorders in Children
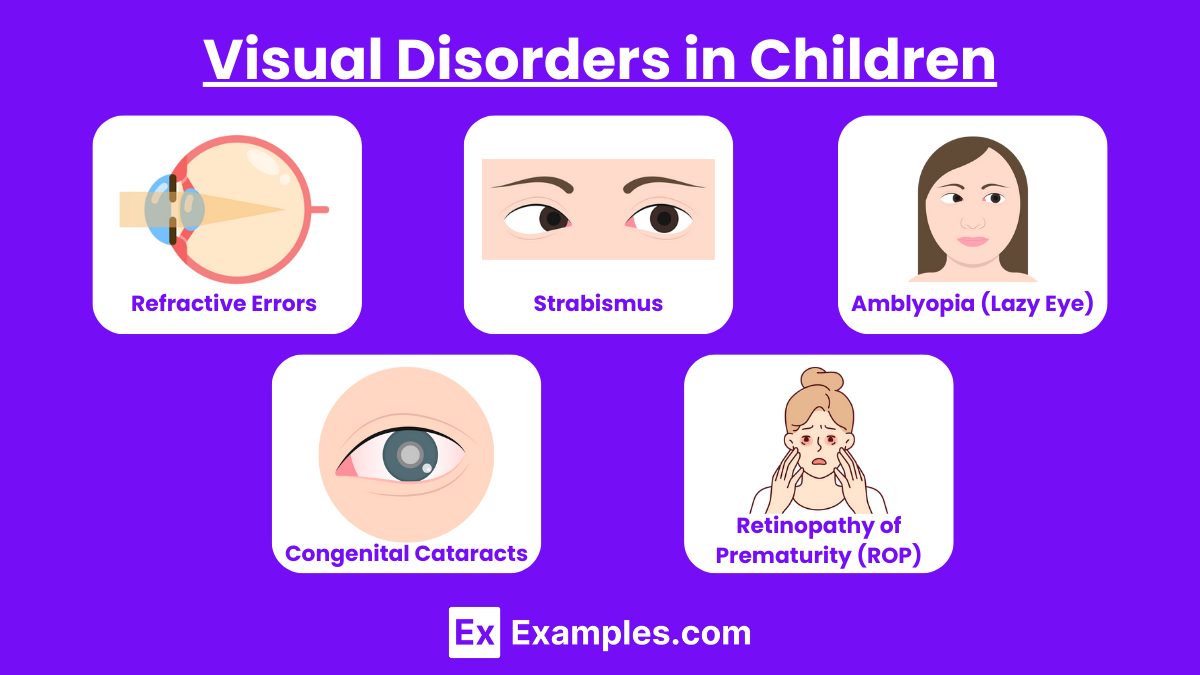
- Refractive Errors : Refractive errors are the most common visual disorders in children, resulting from the eye’s inability to focus light correctly onto the retina. Types include myopia (difficulty seeing distant objects), hyperopia (difficulty seeing near objects), and astigmatism (blurred vision due to an irregularly shaped cornea). These conditions often cause symptoms like squinting, eye strain, or headaches. Diagnosis typically involves vision screening tests such as the Snellen chart or refraction tests. Treatment usually includes corrective eyeglasses or contact lenses. Nurses play a vital role in educating families about the importance of routine eye exams and ensuring children adapt to corrective devices effectively.
- Strabismus : Strabismus occurs when the eyes do not align properly, causing one eye to turn inward (esotropia) or outward (exotropia). This condition can lead to issues with depth perception and, if untreated, may result in amblyopia (lazy eye). Symptoms include misaligned eyes and difficulty focusing. Diagnosis involves tests such as the corneal light reflex and cover-uncover test. Treatment options include patching the stronger eye to encourage use of the weaker one or corrective surgery in severe cases. Nurses should educate parents about patching techniques and emphasize the importance of follow-up care.
- Amblyopia (Lazy Eye) : Amblyopia, commonly known as lazy eye, is characterized by reduced vision in one eye due to poor brain-eye coordination. It often stems from untreated refractive errors, strabismus, or congenital cataracts. Children may experience eye strain, squinting, or a noticeable difference in visual acuity between the eyes. Early diagnosis through visual acuity testing is critical. Treatment involves patching the stronger eye to stimulate the weaker one, corrective lenses, or vision therapy. Nurses play an essential role in educating families on the importance of early intervention and adherence to treatment to prevent permanent vision loss.
- Congenital Cataracts : Congenital cataracts involve clouding of the eye’s lens present at birth, potentially impairing vision development. Causes include genetic factors, maternal infections during pregnancy, or metabolic conditions. Symptoms often include a white reflex in the pupil (leukocoria) and nystagmus. Diagnosis is confirmed through the absence of the red reflex during eye exams. Treatment typically involves surgical removal of the cataract, followed by the use of corrective lenses or intraocular implants. Nurses provide support by educating families on postoperative care, monitoring for complications, and encouraging adherence to follow-up appointments.
- Glaucoma in Children : Glaucoma in children, also known as pediatric glaucoma, is a group of eye disorders that damage the optic nerve due to increased intraocular pressure (IOP). It can be congenital (present at birth) or develop during childhood. Symptoms include excessive tearing, light sensitivity (photophobia), an enlarged cornea, or a cloudy appearance in the eyes. Untreated, it can lead to vision loss or blindness. Diagnosis involves measuring IOP, examining the optic nerve, and assessing the cornea using tools like tonometry and gonioscopy. Treatment often includes medications to lower IOP, laser therapy, or surgical procedures. Nurses play a crucial role in educating families about early detection, adherence to treatment, and the importance of routine follow-up to manage the condition effectively and preserve vision.
Auditory Disorders in Children
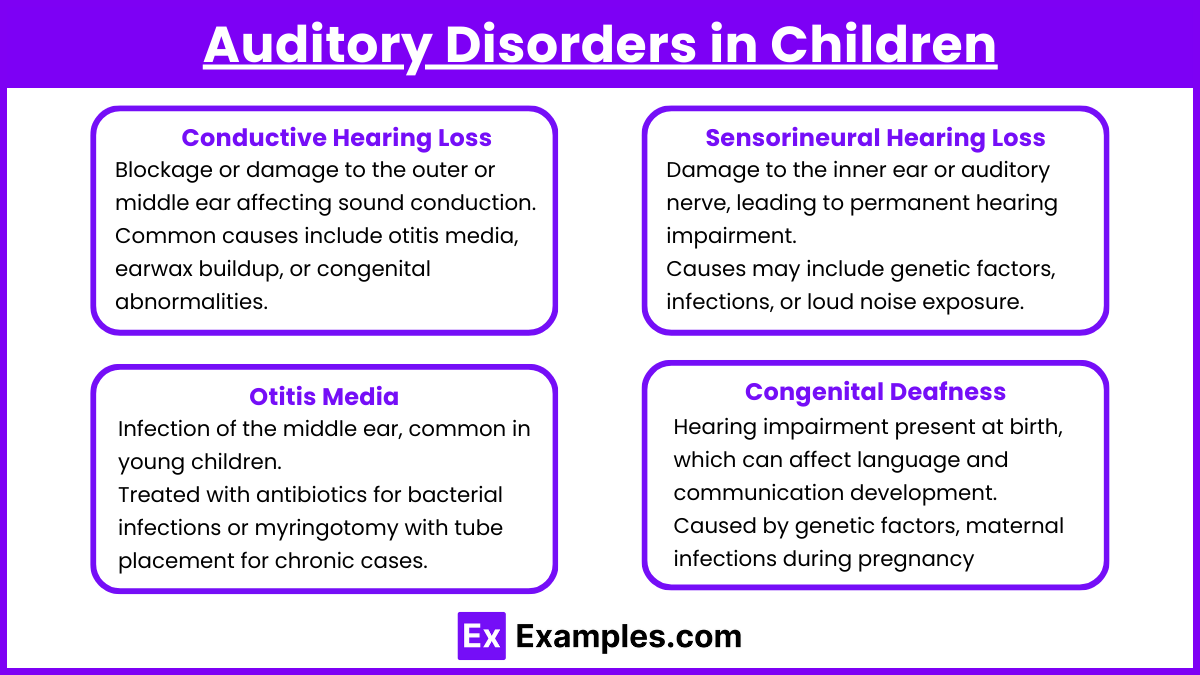
- Conductive Hearing Loss
- Blockage or damage to the outer or middle ear affecting sound conduction.
- Common causes include otitis media, earwax buildup, or congenital abnormalities.
- Managed by removing the obstruction or using hearing aids.
- Families should be educated about proper ear hygiene and encouraged to follow up on care for ear infections.
- Sensorineural Hearing Loss
- Damage to the inner ear or auditory nerve, leading to permanent hearing impairment.
- Causes may include genetic factors, infections, or loud noise exposure.
- Treatment options involve cochlear implants for severe cases and hearing aids for mild-to-moderate hearing loss.
- Early hearing screenings are crucial, and families should be educated about assistive devices and available communication resources.
- Otitis Media
- Infection of the middle ear, common in young children.
- Symptoms include ear pain, fever, irritability, and pulling at the ears.
- Treated with antibiotics for bacterial infections or myringotomy with tube placement for chronic cases.
- Parents should be taught to recognize early symptoms and the importance of completing prescribed antibiotics.
- Congenital Deafness
- Hearing impairment present at birth, which can affect language and communication development.
- Caused by genetic factors, maternal infections during pregnancy (e.g., rubella), or trauma during delivery.
- Management involves a multidisciplinary approach with speech therapy, hearing aids, or cochlear implants.
- Families should have access to early intervention programs and be encouraged to consider sign language or other communication aids.
Developmental Considerations
Visual Development
- Newborns: Vision is limited to about 8-12 inches from their face. They prefer high-contrast patterns, such as black-and-white designs, and are sensitive to bright light. Their ability to focus and coordinate eye movements is not fully developed.
- 1-3 Months: Babies begin to track moving objects and develop better focus, especially on faces. Smiles may be triggered as they start recognizing familiar faces.
- 4-6 Months: Depth perception improves, and babies can focus on objects both near and far. They also begin to develop hand-eye coordination, which allows them to reach for and grasp objects.
- By 6 Months: Babies can focus and track objects more consistently, and color vision is nearly at adult levels. They start showing interest in bright and colorful toys.
- 9-12 Months: Improved eye coordination enables them to judge distances more accurately, helping with crawling and walking.
- Nursing Tip: Encourage parents to engage in activities that promote visual development, such as using brightly colored toys, playing peek-a-boo, and offering safe objects for reaching and grasping. Recommend routine eye exams to detect any abnormalities early.
Auditory Development
- Newborns: Babies can startle at loud noises, indicating an intact auditory reflex. They prefer soothing voices, especially their mother’s, and may quiet down when spoken to.
- 1-3 Months: Infants begin to respond to familiar voices and sounds by cooing or smiling. They can recognize the direction of sound but may not consistently turn toward it.
- 4-6 Months: Babies can consistently turn toward sounds, showing improved auditory localization. They start babbling and experimenting with sounds, laying the foundation for speech development.
- 7-9 Months: Infants become more responsive to their name and begin recognizing tone changes in voices. They may show fear or excitement depending on the pitch or volume.
- By 12 Months: Babies start saying their first words and can imitate sounds. They enjoy music and rhythmic patterns and begin responding to simple verbal commands like “no” or “come here.”
- Nursing Tip: Reinforce the importance of regular auditory screenings at well-child visits. Encourage parents to talk, sing, and read to their child frequently to stimulate auditory and language development. Highlight the significance of addressing any concerns about delayed speech or hearing responses promptly.
Examples
Example 1: Management of Strabismus
A 3-year-old child is diagnosed with esotropia (inward turning of the eye). The NCLEX question may ask about the nurse’s role in implementing the prescribed treatment, such as patching the stronger eye for several hours daily to strengthen the weaker one. Additionally, questions might explore how the nurse should educate parents on recognizing the signs of worsening alignment or complications.
Example 2: Otitis Media Intervention
A 2-year-old presents with ear pain, fever, and tugging at their ear, suggestive of acute otitis media. NCLEX questions may focus on priority nursing actions, such as administering prescribed analgesics, educating parents about completing a full course of antibiotics, or recognizing the need for surgical interventions like myringotomy for recurrent infections.
Example 3: Congenital Hearing Loss Diagnosis
A newborn fails an initial hearing screening in the hospital. The NCLEX could test the nurse’s understanding of early intervention, including referrals for diagnostic audiology testing and resources for family support. Questions might also address the importance of multidisciplinary care, such as incorporating speech therapy and assistive devices like hearing aids or cochlear implants.
Example 4: Refractive Error in a School-Age Child
A 7-year-old struggles academically due to undiagnosed myopia (nearsightedness). NCLEX questions may focus on recognizing symptoms like squinting or sitting close to the board, teaching parents about the importance of routine vision checks, and explaining the use of corrective lenses to improve learning and daily functioning.
Example 5: Retinopathy of Prematurity (ROP) in a Preterm Infant
A premature infant receiving oxygen therapy is at risk for ROP. NCLEX questions may evaluate the nurse’s role in preventing this condition by maintaining optimal oxygen saturation levels, ensuring timely ophthalmologic exams, and supporting parents in understanding the importance of follow-up care to prevent potential vision loss.
Practice Questions
Question 1
A 2-year-old child is diagnosed with strabismus. What is the priority nursing intervention to assist in managing this condition?
A. Refer the child for surgery immediately.
B. Educate the parents about patching the stronger eye.
C. Advise the parents to wait until the child is older for treatment.
D. Encourage the use of corrective lenses only.
Answer: B. Educate the parents about patching the stronger eye.
Explanation:
- Strabismus involves misalignment of the eyes, which can lead to amblyopia (lazy eye) if untreated. The primary treatment includes patching the stronger eye to force the weaker eye to work harder, thereby improving its function.
- Option A: Surgery may be needed, but it is not the first-line intervention.
- Option C: Waiting can worsen the condition as early intervention is critical.
- Option D: Corrective lenses may help, but they are often used in combination with patching for optimal results.
Question 2
A nurse is assessing a 4-month-old infant. Which finding suggests a potential auditory impairment that requires further evaluation?
A. The infant startles in response to loud noises.
B. The infant does not turn toward sounds.
C. The infant coos and babbles during interaction.
D. The infant responds to their name being called.
Answer: B. The infant does not turn toward sounds.
Explanation:
- By 4 months of age, infants should demonstrate a behavioral response to sound, such as turning their head toward a noise source. A lack of response suggests a potential auditory impairment.
- Option A: Startling to loud noises is a normal newborn reflex and does not indicate hearing loss.
- Option C: Coos and babbles are normal developmental milestones and do not indicate impairment.
- Option D: Responding to their name typically occurs closer to 6 months or older.
Question 3
The parents of a newborn ask about the causes of retinopathy of prematurity (ROP). Which statement by the nurse is most accurate?
A. “ROP is caused by an infection acquired during delivery.”
B. “ROP is due to abnormal blood vessel growth in the retina.”
C. “ROP occurs because of excessive exposure to sunlight after birth.”
D. “ROP results from genetic factors passed down from parents.”
Answer: B. “ROP is due to abnormal blood vessel growth in the retina.”
Explanation:
- Retinopathy of prematurity (ROP) is a condition primarily affecting premature infants. It occurs due to abnormal vascular growth in the retina, which can lead to scarring and retinal detachment if untreated.
- Option A: ROP is not caused by infections.
- Option C: Sunlight exposure is unrelated to ROP.
- Option D: While genetics may play a minor role in some eye conditions, ROP is more commonly linked to prematurity and high oxygen therapy.